I had been warned—I found it hard to believe—that WHO ministerial meetings can be rather dull affairs of little consequence. Ministers typically take it in turn to read their prepared speeches; their fellow ministers appear to be listening attentively through their headsets but some, it seems, have been known to zap through the simultaneous translation channels in search of lighter entertainment. Speeches aren’t played over the loudspeakers for fear of waking jetlagged ministers from their afternoon naps. WHO is a very considerate organization: it likes to make sure that while on its premises visitors reach “a state of complete physical, mental and social well-being.”
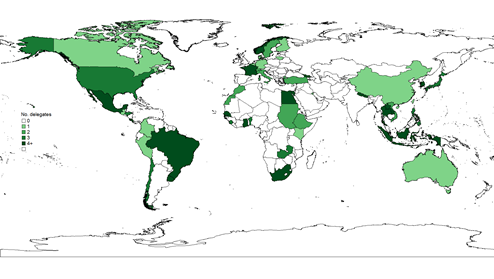
Well I’m happy to report that last week’s ministerial meeting on Universal Health Coverage (UHC)—held in Geneva on February 18-19, jointly organized by WHO and the World Bank, and attended by delegates from all over the world (see map)—didn’t fit the stereotype.
The sister act  I suspect this had something to do with the fact that two formidable women, WHO’s Margaret Chan and the World Bank’s Tamar Manuelyan Atinc (they call one another “sisters”) chaired most of the sessions. Between them they set a cracking pace, politely but firmly keeping everyone in line. They set the facilitators free to pace athletically around their central enclosure quizzing ministers and UN ambassadors, interrupting anything that looked like a set speech.
I suspect this had something to do with the fact that two formidable women, WHO’s Margaret Chan and the World Bank’s Tamar Manuelyan Atinc (they call one another “sisters”) chaired most of the sessions. Between them they set a cracking pace, politely but firmly keeping everyone in line. They set the facilitators free to pace athletically around their central enclosure quizzing ministers and UN ambassadors, interrupting anything that looked like a set speech.
 For the most part, the ministers and ambassadors seemed to like these new punchier rules of engagement. There were fun moments, and some slightly offbeat ones too. The Samoan Minister of Finance recounted how Samoa had recently changed its time zone. “We were the last country in the world to see the sun set. Now we are the first to see it rise.” There was a lot of chumminess. Finance and health ministers smiled at one another. Several finance ministers actually said they had every confidence in the health ministry. (In my country when the prime minister says that of a minister she’s actually about to fire him.)
For the most part, the ministers and ambassadors seemed to like these new punchier rules of engagement. There were fun moments, and some slightly offbeat ones too. The Samoan Minister of Finance recounted how Samoa had recently changed its time zone. “We were the last country in the world to see the sun set. Now we are the first to see it rise.” There was a lot of chumminess. Finance and health ministers smiled at one another. Several finance ministers actually said they had every confidence in the health ministry. (In my country when the prime minister says that of a minister she’s actually about to fire him.)
#UHC we can!
There are a couple of features of WHO ministerial meetings that are apparently hard to change. Technical people are to be seen but not heard at these meetings, rather like children who are allowed to stay up after bedtime to see their parents welcome their guests to a dinner party. Many of us resorted to Twitter, broadcasting in real time to the outside world in 140 characters or less everything that seemed newsworthy; the number of tweets mentioning #UHC spiked on the days of the conference thanks to our efforts (see chart). The other immutable feature of WHO ministerial meetings is the absence of real debate: however hard they tried, the moderators rarely got the delegates to disagree with one another. Some of us used Twitter to debate issues among ourselves and with anyone who was online and following our tweets; flash points included the roles of voluntary insurance and the private sector. 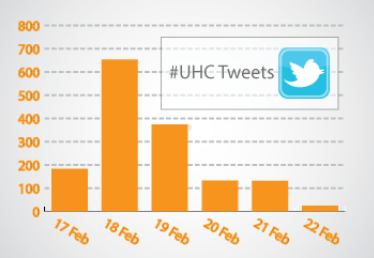
So what did we learn?
Delegates expressed support for the ideas underlying UHC—that everyone, irrespective of their ability to pay, should have access to the care they need, without putting their family at financial risk. As Ms Manuelyan Atinc put it, “No one should have to choose between the health care they need and feeding their families.” Dr Chan, citing the Lancet, said UHC is “sweeping the globe, changing how health care is financed and how health systems are organized.” South Africa injected a sense of realism into the proceedings: “UHC is an orientation not a destination.” it warned.
Many delegates spoke of the importance of getting political commitment to UHC at the highest level. South Africa said that a strong partnership between the MOF and MOH is essential: “In South Africa”, the delegate said, “the two ministries now dance together.”
Several countries, including Morocco and Nepal, spoke of their decision to focus their limited resources initially on the poor and vulnerable. In her closing remarks, Ms Manuelyan Atinc expressed her approval of this approach, but urged health ministries to work closer with social affairs ministries to ensure consistency of targeting efforts across social programs. Delegates also spoke of the need to be realistic about what could be covered initially.
How to finance UHC was a common theme. Marie-Paule Kieny from WHO reminded everyone that UHC isn’t just about formal health insurance; taxes and other forms of government revenue also contribute to financial risk protection. With the exception of Senegal, there was little talk of voluntary insurance being a serious choice along the road to UHC. Ghana reminded us that despite its name the National Health Insurance Scheme is largely tax-financed. A recurring theme was how to raise additional revenues to expand and deepen coverage. Ghana’s scheme has a chronic deficit, forcing the government to think of raising the VAT rate. The Philippines is introducing a sin tax on tobacco and alcohol, and is earmarking revenues for an expansion of PhilHealth coverage, beginning with the poor and vulnerable.
There was agreement that human resource shortages posed a challenge. The international brain drain was discussed, with fingers pointed at certain rich countries that are proving popular destinations for medical migrants. The US outlined its efforts to reduce its demand for medical migrants and its efforts to help build more capacity in the developing world. Dr Chan commended the UK for its efforts to stem the tide of medical migration to the UK. Brazil urged delegates to think not just about the overall number of health workers, but also their distribution, especially between poor and more affluent areas.
Several delegates argued—especially those representing finance ministries—that the health sector could do much more with existing resources. The Nepal delegate argued for “spending wisely, not widely”. Improving information systems was a common theme. “Without such improvements”, Colombia said, “it’s hard to ensure that government funds are actually used on delivering necessary patient care.” Chile told delegates that its experience had shown that strong accountability and a good information system are both essential to ensuring results. Mexico outlined new rules that will force states to be more accountable to the center for its federally-funded health spending. Morocco pointed to the need for strong accountability to reduce waste and ensure quality care for everyone. Several delegates highlighted the need to provide providers with the right incentives. Georgia said it is moving to DRGs and introducing quality assurance programs.
There seemed to be some disagreements beneath the surface about the role of the private sector in delivering publicly-financed care. Dr Chan spoke of the trust the public sector enjoys but its poor record on efficiency. The finance ministry delegate from the Philippines noted that there privatization of water and power had resulted in improvements in service delivery. “Shouldn't the government explore contracting with the private sector?” he asked. Someone pointed out that Japan had achieved UHC with 70% of care provided by private sector.
The importance of data and monitoring progress towards UHC was a recurrent theme. " Ghana spoke eloquently of the country's culture of use of data and evidence to promote accountability in the drive toward UHC. The Philippines said it would judge the success of the sin tax reform in terms of lives saved and the health improvements, adding that metrics are essential to ensure that UHC initiatives don’t become “a black hole”. South Africa said it was putting quality at the center of its UHC agenda, and said the government wants to know whether mortality and morbidity will improve as a result of UHC. Zambia said it wanted evidence specifically on the impacts of UHC initiatives, not just of the health system in general. Josep Figueras, one of the facilitators, asked how in monitoring progress toward UHC we could balance richness of UHC and the need for simplicity. He urged us to “avoid paralysis by analysis.
Inevitably the role of UHC in the post-2015 agenda came up. In the shortest intervention of the meeting, Turkey encouraged all to place UHC at center of post-2015 development goals, and said it would like to work with other countries on this agenda. The US concurred that UHC could be the unifying post-2015 health development goal. Closing the meeting, Ms Manuelyan Atinc said she too agreed but suggested that there should be an overall health outcome goal too, like healthy life expectancy. “Better health is, after all, what we’re all about.” she reminded us.


Join the Conversation