For several decades, Bangladesh has been combatting communicable diseases with variable success. While this fight is not yet finished, the country is now faced with yet another alarming challenge: noncommunicable and chronic diseases, which account for 68% of deaths in the country.
A recent World Bank study reports that, among 23 developing countries, Bangladesh ranks ninth in rates of mortality due to chronic diseases, primarily cardiovascular diseases (CVDs), cancer, respiratory diseases, injuries, and diabetes. A study in medical college hospitals found that about one-third of hospital admissions in patients aged 30 years and over were due to major NCDs. As shown in Figure 1, CVDs alone account for about 16% of total deaths.
Figure 1. Leading Causes of Mortality and Morbidity in Bangladesh, 2010 Estimates
Source: Institute of Health Metrics & Evaluation (2013)
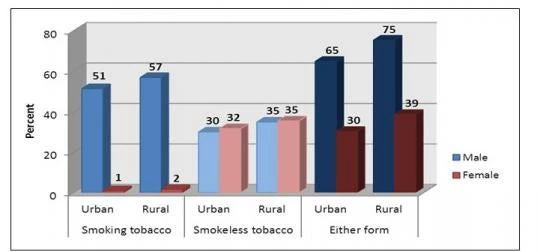
Aside from injuries, all are linked to a few common risk factors—high tobacco use, air pollution (including indoor fires for cooking and heating), poor diet and nutrition, occupational risks, high blood pressure, malnutrition and low birth weight, and lack of physical activity. Among adult males, 65% of urban residents and 75% of rural residents use a form of tobacco (Figure 2).
Figure 2: Tobacco Use among Adults of 25 Years and Above by Locality, Bangladesh, 2010
Source: WHO Bangladesh 2011
With other social determinants such as poverty, low education, urbanization, and changing lifestyles, the risk of NCDs rises. These factors have long-lasting, transgenerational impacts, particularly on the poor. For example, for low-income groups, direct costs associated with diabetic care could drain up to 24.5% of annual household income.
In addressing the challenges of the Millennium Development Goals, the health service delivery system in Bangladesh—as in most developing countries— was structured to deal with “episodes” of maternal and child health illnesses and communicable diseases. As the disease burden shifts, so must the country’s health system to ensure continuity of care, more focus on prevention, coordination across sectors, and a stronger regulatory framework.
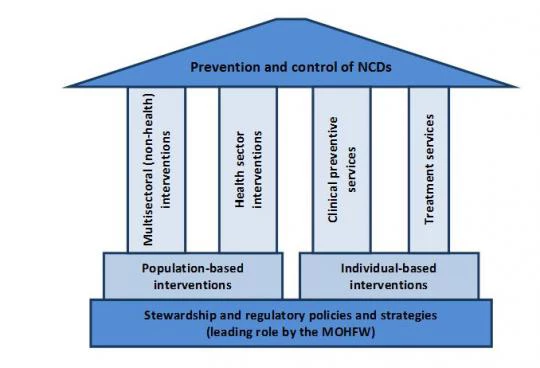
Tackling NCDs comprehensively would require the adoption of an integrated approach to mobilize the different sectors of the government, as well as forging a partnership between public and private sectors. Figure (3) represents a framework for policy options related to NCDs.
Figure 3: A Policy Options Framework for the Prevention and Control of NCDs
The framework is founded on a “stewardship and regulatory” role, which should be led by the health sector, represented by the Ministry of Health, and should include mobilizing the non-health sector. Population-based and individual-based policy interventions are grounded on four pillars: multisectoral and health sector interventions, and clinical preventive and treatment services.
Each policy intervention mobilizes different parts of the health and non-health sectors and requires very different inputs in infrastructure, capacity, and skill sets, while yielding very different outputs and outcomes. Harmonizing both sets of policy interventions is necessary to ensure a “strategic mix” so that population-based policy interventions complement those delivered to individuals within the clinical care system.
A key initial challenge is to determine the strategic priorities that will constitute the building blocks in the short and medium term. Given the impoverishing effect of NCDs and their ever-increasing costs, the government should consider these priorities in the context of poverty reduction and reducing upward pressure on public finance. Operationally, it is important to capitalize on current activities and take into account available resources. In addition, these strategic priorities should be selective in terms of considering mainly the most common risk factors—namely, high blood pressure, high tobacco use, unhealthy diet, malnutrition and low birthweight, and arsenic in water sources.
The Ministry of Health, for the health sector, will have the leading role in these strategic priorities, which will require full integration in the relevant operational plans. Ministry staff will also need new skills to work effectively with other sectors, to build a multisectoral alliance to ensure synergy.
Follow the World Bank health team on Twitter: @worldbankhealth.
Related
Report: Tackling Noncommunicable Disease in Bangladesh: Now Is the Time
World Bank and Health



Join the Conversation