A recent study on patient safety in Kenya revealed that less that 5% of health facilities, both public and private, have attained the minimum international standards of safety. Although such studies are rare, there is reason to believe that the same picture prevails in most of SS Africa.
In Kenya, and especially following the enactment of a new constitution, which gives all Kenyans the right to access quality care and free access to emergency services, there has been an unprecedented increase in media coverage of medical malpractice complaints from the public, ranging from clinical care processes gone wrong to complaints of outright unethical practices and behaviours. The media coverage is merely a response to an increased public awareness, concern about and demand for information on how the health system is performing, and an interest in knowing what those in authority are doing to ensure that health services are provided in a safe and humane manner.
As a result, the Kenya Medical Practitioners and Dentists Board (KMPDB) and other regulators have had to constantly engage the media to respond to complaints and explain what it is doing to dispense justice and improve the situation.
This sudden demand to detailed information on malpractice cases would put any health regulator under massive pressure, especially considering that healthcare providers in most of Africa have largely remained autonomous, with little scrutiny from the public.
However, KMPDB has so far responded to these reports with clarity, thanks to an earlier collaborative effort with the World Bank Group’s (WBG) Health in Africa Initiative. The Board has taken time to explain the nature and characteristics of the cases, and outlined mechanisms that have been put in place to streamline the processes and protect both the public and the practitioners.
The Board’s engagement with the WBG started in 2012, when the Board asked for the World Bank Group (WBG) to help streamline the medical malpractice system. Prior to that, there was no formalized mechanism for classifying and tracking malpractice cases from the time of reporting to conclusion, yet there was evidence that the frequency of complaints was increasing.
The WBG agreed to: one, review and fairly/justly conclude the backlog of 736 cases dating back 15 years, and give recommendations on processing of future cases; and two, analyse the case patterns and malpractice processes and develop recommendations on changing the reporting and processing systems to make them more responsive to the public. The two activities would culminate in the development of a new framework for receiving, processing and reporting medical malpractice claims.
As a result, the Board and the WBG developed a report showing the nature and characteristics of past malpractice complaints and recommending an appropriate classification system based on past experiences; a framework for receiving, processing and reporting malpractice complaints, all linked to other Board functions, including licensing and the implementation of Continuous Professional Education; and finally, proposals for amendments to the Disciplinary Rules; Assessment, Training and Registration Rules; and Inspections and Licensing Rules under the Medical Practitioners and Dentists Act. The proposals were subsequently drafted and gazetted under the Medical Practitioners and Dentists Act.
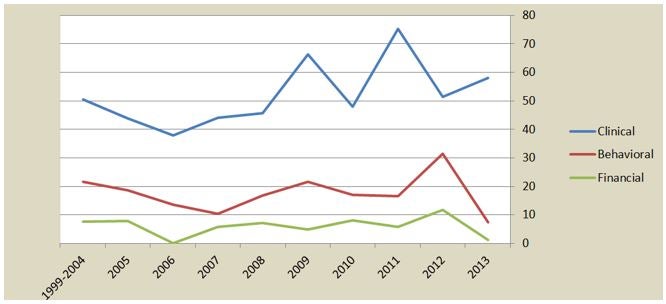
Trends in malpractice complaints lodged at MPDB between 1999 and 2013
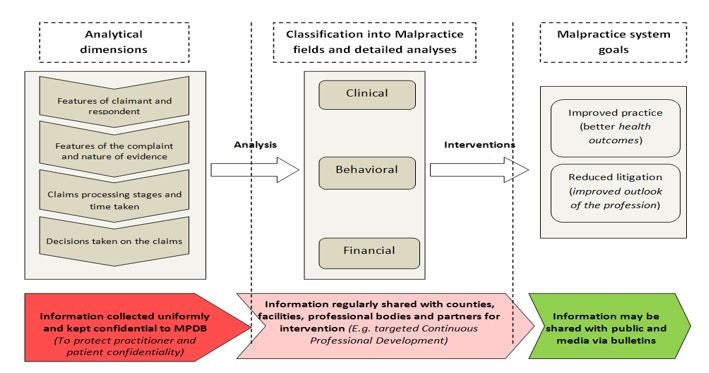
Framework proposed and adopted by MPDB for collection, processing and reporting of malpractice cases
The next steps will include automating the malpractice system to, not only expedite the processes for swift justice, but also create a platform that can allow the Board to monitor complaint patterns, and institute timely remedial measures. This is important for Kenya and other African countries, where complaints against healthcare providers are on the rise. Failure to monitor and resolve cases in good time could result in clients seeking redress through the judiciary, which could increase medical indemnity insurance, with a consequent rise in costs of healthcare. In addition, having an automated system makes it possible to share some information with the public, which increases confidence in the grievance redress system and promotes social accountability.



Join the Conversation