 Micronesia, WHO
Micronesia, WHO
This blog is part of a series on Universal Health Coverage (UHC). The series includes contributions from external bloggers and reflects their views. Follow the conversation on Twitter #HealthForAll.
In Metamorfosi, Greece an 80 year-old man, Pantelis Leosis, is grateful that his new local health clinic is a ten-minute drive away. “I found a setting that was very friendly and pleasant. I definitely don’t pay anything,” he said. This primary health care (PHC) service has transformed how he receives treatment for his heart condition.
In just one year, Greece has established nearly 100 new community-based primary health units, free at the point of access and known locally as Topikes Monades Ygias or TOMYs. In a few months, around a million people will benefit from the new services. The units are the key elements of the newly designed primary health care system and are the first point of contact and the main component of healthcare services for people in the area. WHO worked with the Greek Ministry of Health to support the rollout of this nationwide PHC effort.
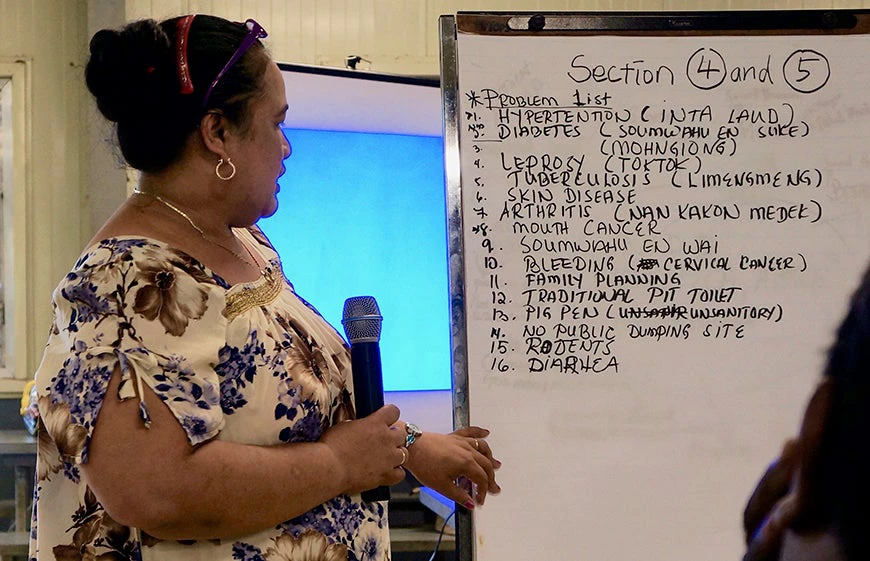
A primary health care approach is also helping ensure that Micronesia's 100,000 people – scattered across hundreds of islands in the Pacific Ocean – are able to receive a comprehensive package of care spanning the life course. The Dispensary Strengthening Programme brings health workers to remote communities to provide comprehensive outreach services to tackle a variety of health needs including screening for non-communicable diseases, tuberculosis, leprosy and cervical cancer; health education; basic treatment; and dispensing of medications.
The programme also collects biometric data, which is shared with drug dispensary and hospital information systems, to support continuity of care and follow-up. The Department of Health Services of Pohnpei State leads the programme with support from the national government, the World Health Organization (WHO), the International Organization for Migration, the Japan International Cooperation Agency, and the Island Food Community of Pohnpei.
It is clear that primary health care reforms are transforming how populations can access health services, an approach which is fundamental to how the world will achieve universal health coverage (UHC).
To build and strengthen a health system that can deliver UHC to its population takes careful consideration of where and how to put resources and take action. A country’s health system and UHC must be supported by a whole range of institutions across sectors, communities and people, with structures put in place to ensure UHC is sustainable.
This is, of course, no easy task and takes time; yet the sense of urgency is growing. Current funding levels around the world are insufficient to achieve UHC by 2030 and must increase. It is also critical to ensure the process is country-owned and actions are implemented in collaboration with a range of stakeholders.
The approaches that WHO take to achieve UHC strive for both co-construction and longevity. In many countries, WHO is working with a range of Ministries, development partners, non-governmental and community organizations among others to strengthen health systems, legal frameworks and community engagement to deliver UHC. WHO works jointly with national and international partners on PHC to support country priorities through established national mechanisms such the health sector coordination committee. WHO is also currently working jointly with UNICEF to implement the post- Astana PHC agenda.
The more we work to put the right structures in place, the faster we will make progress towards the triple billion goals as laid out in the WHO 13th General Programme of Work 2019-2023: 1 billion more people benefiting from universal health coverage, 1 billion people more people better protected from health emergencies, and 1 billion more people enjoying better health and well-being. And the faster we will make progress towards achieving SDG3 and UHC.
Primary health care is a cornerstone for UHC. Legal reform is another core area, which embeds sustainability and longevity into UHC. The Philippines has just signed a Universal Health Care Bill into law that automatically enrolls all Filipino citizens in the National Health Insurance Program and prescribes complementary reforms in the health system. In 2016, 54% of healthcare spending was paid out-of-pocket. When implemented effectively, the Act will mean all Filipinos get the health care they need, when they need it, without suffering financial hardship as a result. The UHC Act was carried by a broad coalition of parliamentarians across the political spectrum. WHO advocated and informed the consultation and drafting process of the Bill in the Senate during the second half of 2017, gently steering the process in the areas of people-centred integrated service delivery and health financing.
Citizens and communities must also be at the heart of any transformation in health systems and services. Tunisia has organised a series of engaging meetings between government representatives, civil society organisations and citizens eager to discuss and make decisions about the national health policy. Finding common ground on health policy issues and ways to make progress will result in a stronger national health system in line with the aspirations of its citizens and will substantially improve the health of Tunisian citizens. The Tunisian Ministry of Health, with support from WHO's UHC-Partnership, have so far organised two phases of the Societal Dialogue for health system reform.
These examples are very different and all show that putting resources into the right places, in the right context and at the right moment are crucial for UHC. Strong and sustained action adapted to the context is key. The task ahead of us – to achieve UHC by 2030 – might seem daunting, but with reforms and resources directed to the right areas and focused on Primary Health Care, there is hope that everyone, everywhere will enjoy the right to health.



Join the Conversation