
Five billion people—two thirds of world population—lack access to safe and affordable surgical, obstetric and anesthesia care with low and middle income countries (LMICs) taking a lead.1-3 Surgical care is a crucial component of building strong health systems and one that is often overlooked (Dr. Jim Kim UHC 2017 video). All people are entitled to quality essential health services, no matter who they are, where they live, or how much money they have. This simple but powerful belief underpins the growing movement towards universal health coverage (UHC), a global commitment under the Sustainable Development Goals (SDGs). Inherent in the framework of UHC is access to safe surgical, obstetric and anesthesia (SOA) care.
An estimated 33 million undergo financial hardship every year from the direct costs of surgical care. And those are the individuals fortunate enough to have access to care.4 Moreover, about 11% of the world’s disability-adjusted life years are attributable to diseases that are often treated with surgery such as heart and cerebrovascular diseases, cancer, and injuries from road traffic accidents.2,5 Other surgically treatable disorders such as obstructed labour, obstetric fistulas, and congenital birth defects are major causes of morbidity and mortality in the developing world.5,7 The delivery of safe and quality SOA care is critical for the realization of many of the Sustainable Development Goals, including: Good health and well-being (Goal 3); No poverty (Goal 1); Gender equality (Goal 5), and Reducing inequalities (Goal 10).
When discussing surgery in the global health arena, it is important to remember that we are referring not to the surgeon, obstetrician or anesthetist, but the patient undergoing a surgical procedure, and the many different processes, places, infrastructures and personnel involved in that journey. From the identification of surgical diseases in the community, through to the hospital facility, blood transfusion laboratories, antibiotic prophylaxis, anesthetic equipment and postoperative wound care and complications, surgical care is many-layered and heavily embedded within the secondary and tertiary healthcare facility.
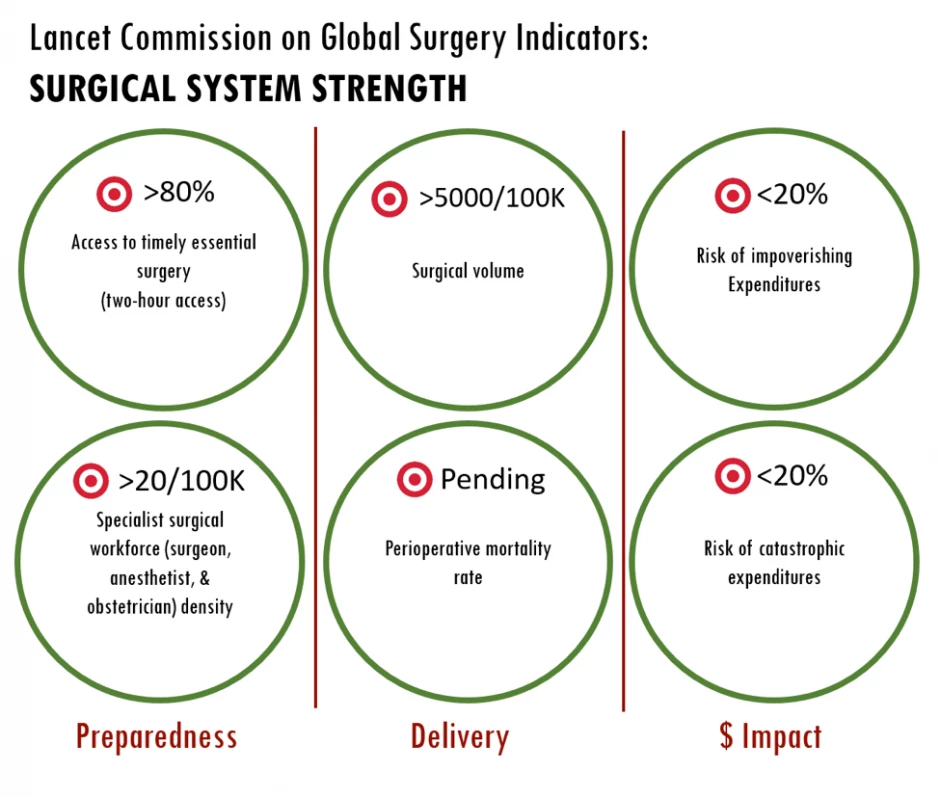
Data drive quality improvement processes in business and health systems in high-resource settings, but to date, information on the surgical burden of disease in LMICs has been severely limited by gaps in national data and a paucity of standardized definitions for tracking surgical services globally. To address this lack of knowledge, Dr. Jim Kim challenged the Lancet Commission on Global Surgery (LCoGS) in 2014 to develop consensus-based indicators and time bound targets to track progress.8 In a global consultative process with partners in over 110 countries, the commissioners published “Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic growth” in 2015.2 In this report, the commissioners presented six core indicators aiming to evaluate the strength of a surgical system.
Six core indicators of surgical system strength
These indicators are:
- Access to timely essential surgery: The proportion of the population in each country that can reach, within two hours, a facility capable of providing caesarian section, laparotomy, and treatment of open fracture (the Bellwether Procedures).
- Specialist surgical workforce density (WDI indicator SH.MED.SAOP.P5): The number of specialist surgical, anaesthetic, and obstetric (SAO) providers who are working in each country per 100,000 population.
- Surgical volume (WDI indicator SH.SGR.PROC.P5): The number of procedures undertaken in an operating theatre per 100,000 population per year in each country. A procedure is defined as the incision, excision, or manipulation of tissue that needs regional or general anaesthesia, or profound sedation to control pain.
- Perioperative mortality rate: The number of in-hospital deaths from any cause in patients who have undergone a procedure done in an operating theatre, divided by the total number of procedures, presented as a percentage.
- & 6. Risk of impoverishing (SH.SGR.IRSK.ZS) and catastrophic (SH.SGR.CRSK.ZS) expenditure for surgical care: The probability of experiencing impoverishment (using a threshold of $1.25 PPP/day) when surgical care is required and the probability of experiencing catastrophic expenditure (10 percent of total income) when surgical care is required.
Together, these indicators and time-bound targets allow a thorough assessment of the strengths and weaknesses of surgical systems, highlighting opportunities for improvement for key stakeholders.
A global data collection effort, but some data remain scarce
After the publication of the LCoGS report, a team of 18 researchers based at Harvard University in Boston began to collect nationally-representative data for each indicator in the 215 countries and independent economies recognized by the World Bank. This Global Indicator Data Collection project was the first attempt to systematically and comprehensively gather primary data on surgical systems on a global scale in order to improve on previously modeled estimates.9 The collected data were published and included in the 2015 World Bank Development Indicators.10
In order to assess temporal changes in these indicators, in 2016 the process of collecting these six indicators was repeated; this time led by researchers at King’s College University in London and driven by highly motivated medical students from all corners of the world. Data retrieval process from each of the World Bank’s list of 215 countries and independent economies consisted of thee main strategies: 1) Direct contact with official bodies 2) Systematic reviews of published literature and, 3) Internet searches of the grey literature.
Of the countries that we received recent (less than five years old) data, the indicators 2 “Specialist surgical workforce density” (71 countries) and 3 “Surgical volume” (60 countries) were most commonly reported, whereas data on indicators 1 “Access to timely essential surgery” (33), 4 “Perioperative mortality rate” (29), 5 (16), and 6 “Risk of impoverishing and catastrophic expenditure for surgical care” (16) remained scarce. Although the reported data provides a better picture of the current state-of and disparities-in access to surgical, obstetric and anesthesia care around the world, more accurate data urgently needs to be collected.
The future of surgical data
SOA care is a public health priority. Whilst this new data is a start in the long journey towards having quality, accurate SOA data for all countries around the world, this second round has demonstrated once again the paucity of sources available – locally, nationally and internationally. The challenges include defining what the best method of sampling the quality of surgical systems, as well as the low incentives and weak structures in place to do so. The challenges in collecting these indicators vary across countries, and so as the way to improve data collection systems. Formation, implementation and evaluation of the SOA plan national wise can help in identification may help in the timely and accurately tracking of these data.
Combined and coordinated effort between policymakers, experts, governments, civil society and other stakeholders including trainees is required to make SOA data collection commonplace and sustainable and to improve quality and access to SOA care worldwide.
REFERENCES
- Shrime MG, Bickler SW, Alkire BC, Mock C. Global burden of surgical disease: an estimation from the provider perspective. The Lancet Global health. 2015;3 Suppl 2:S8-9.
- Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-624.
- Alkire BC, Raykar NP, Shrime MG, et al. Global access to surgical care: a modelling study. The Lancet Global health. 2015;3(6):e316-323.
- Shrime MG, Dare AJ, Alkire BC, O'Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. The Lancet Global health. 2015;3 Suppl 2:S38-44.
- Funk LM, Weiser TG, Berry WR, et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet. 2010;376(9746):1055-1061.
- Global Burden of Disease Cancer C, Fitzmaurice C, Dicker D, et al. The Global Burden of Cancer 2013. JAMA oncology. 2015;1(4):505-527.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine. 2006;3(11):e442.
- Keynote Address by Dr. Jim Kim. Available at: http://www.lancetglobalsurgery.org/launch---boston--may-2015. Assessed January 3rd 2018.
- The Lancet Commission on Global Surgery Surgical Indicators Report 2015. Available at: http://www.lancetglobalsurgery.org/indicators. Assessed January 3rd, 2018.
- Ng-Kamstra J., Raykar N., Meara J.G., Shrime M.G. Measuring surgical systems: a new paradigm for health systems strengthening. Worldbank blog. Available at: http://blogs.worldbank.org/opendata/measuring-surgical-systems-new-paradigm-health-systems-strengthening. Assessed January 3rd, 2018.






Join the Conversation