We took over the management of the obstetrics, gynecology, and pediatric hospital in Yaoundé (HGOPY) in 2014, inheriting an institution that faced chronic structural debt, obsolete equipment, and dilapidated buildings. No debt repayment plan was in place and fixed expenses such as staff salaries and benefits were extremely high.

This situation was regrettably common in many institutions across Africa which were hit hard by the economic and social crisis that resulted from structural adjustment policies implemented in by several countries, including Cameroon. Furthermore, the decision to increase health care charges adversely affected the poorest, limiting their access to health care and leading to a rise in maternal and infant mortality rates.
In response, African countries signed the Abuja Declaration in 2000, committing to earmark at least 15% of their national budget to the health sector. In addition to the goal of providing universal health care, the sector was expected to enhance the performance, effectiveness, and efficiency of its services.
Consequently, faced with limited resources, a shortfall in revenue relative to expenditure, and stagnant public subsidies, we had no choice but to rethink the hospital’s management strategy. Following the technical, administrative, and financial audit conducted by the Technical Rehabilitation Committee (CTR), which classified the institution as “a high risk,” we sought the World Bank’s expertise in October 2013.
The Bank noted that the hospital’s monthly structural debt amounted to roughly CFAF 23.2 million. This debt was primarily attributable to all payments to staff (wages and salaries, fixed allowances, social security contributions and matching shares), which accounted for 65% of all expenditure, while in theory, payroll should not exceed 60% of total expenditure.
The World Bank’s study also revealed that the services being offered at the hospital were of poor quality, despite high staffing levels. Medicines and supplies were often not in stock, and there were frequent medical equipment breakdowns, forcing staff to send patients to private institutions.
To address these shortcomings, the World Bank made the following proposals:
- Reduce staff numbers by at least 25% to lower payroll costs;
- Revise the base for calculating wages and salaries. Wages and salaries should include a fixed portion (50%) and a variable portion (50%) corresponding to performance bonuses; and
- Raise awareness among staff about the need for a change in the working methodology and encourage them to improve service quality.
Eager to get things going, while according priority to keeping the communication channels open to maintain a peaceful social climate, and secure the buy-in of all staff, we opted, in the face of skepticism from the World Bank’s expert, to keep the payroll system in place and use our own funds to introduce a performance-based financing (PBF) system.
To achieve this objective, we sent 14 employees to international PBF courses in Limbé and Douala. The remaining staff members were trained at the hospital and awareness raising was provided in weekly meetings. The hospital’s management also organized work sessions with World Bank experts, as well as the Health Sector Support Investment Project (PAISS) team and representatives from the Contracting and Verification Agency (ACV) in Littoral.
In an effort to build a results-oriented team, we merged the existing 28 departments into 14 departments (11 medical and 3 administrative). Each department was free to manage itself as it saw fit, on the technical and administrative fronts. We introduced and applied performance and management indices, which allowed us to compare the departments to determine which ones showed a surplus or a deficit. Team spirit and solidarity were therefore also strengthened.
On April 1, 2015, the radiology department, the clinical biology laboratory, and the ophthalmology unit were selected to pilot this new concept, which was later rolled out in all the other departments. We then conducted a technical quality assessment, drew up business plans, signed performance contracts, prepared statistical tools to measure the indicators, and conducted satisfaction surveys for each department.
Our efforts began yielding positive results quickly. We noted an uptick in revenue and visits; health care services improved and costs were being contained. As a result of staff buy-in, the departments also made significant strides in evaluating their performance.
However, we would never have been able to implement this new approach without a special dispensation authorizing us to bypass normal rules governing hospital management. We were able to exercise autonomy and directly manage the procurement of hospital equipment and supplies, using competitive bidding to secure the best possible price. We were also able to have our performance assessed by external impartial experts, and to conduct a patient satisfaction survey of all our departments, health care services, and practices.
Having quickly realized that we could not closely follow traditional PBF programs, we tailored the approach to the prevailing circumstances in our institution. For example, we had to reach a compromise in order to maintain certain emoluments (staff allowances and wages and salaries), and we were unable to implement the social plan recommended in traditional PBF programs to reduce staffing.
Our experience illustrates the need for increased administrative flexibility and financial autonomy in hospitals. This is how we will make them more efficient vis-à-vis patients, and economically viable.
Chart 1: Revenue earned between April 2014 and March 2015 and between April 2015 and March 2016

An analysis of this chart shows considerably higher revenue since the implementation of the PBF approach.
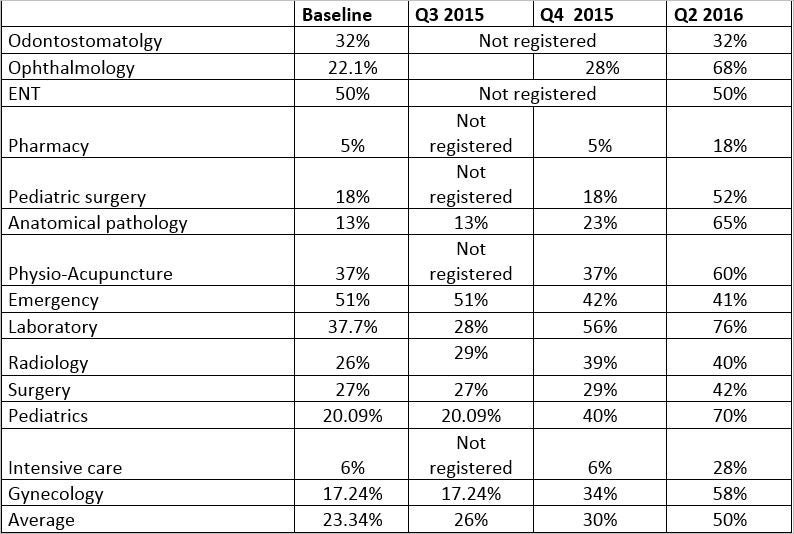
Table 2 : Quality of services under the PBF system between April 2015 and June 2016

Join the Conversation