On February 1st, India’s finance minister presented the Union Budget for 2017-2018, and announced the government’s plan to eliminate tuberculosis (TB) by 2025. This is a welcome move. While ridding people of the burden of any disease is a worthy goal by itself, TB elimination provides perhaps one of the strongest cases for public intervention from an economic point of view.
All communicable diseases present what economists call externalities: infectious people can infect other people who in turn infect others and so on. In fact, economist Phillip Musgrove used TB in particular to illustrate this: “no victim of tuberculosis is likely to ignore the disease, so there is no problem of people undervaluing the private benefits of treatment. Rather, the cost of treatment--and the fact that they may feel better even though the disease has not been cured-- may lead people to abandon treatment prematurely, with bad consequences not only for themselves but for others. The rest of society therefore has an interest in treating those with tuberculosis, and assuming at least part of the cost.” Reducing TB incidence could generate benefits of $33 per dollar spent, prompting The Economist to put TB among their list of ‘no-brainers’. According to the Stop TB Partnership, ending TB globally could yield US$ 1.2 trillion overall economic return on investment.
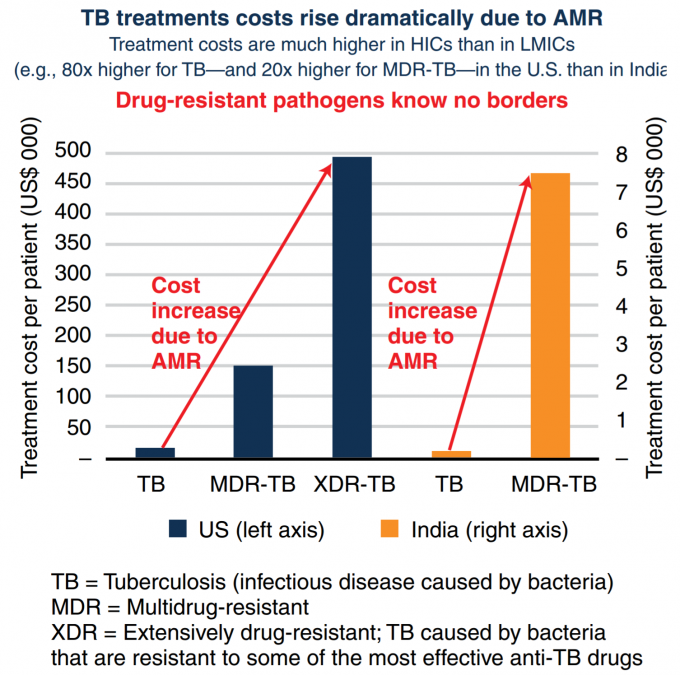
Given the public health importance of TB, all governments must take an active interest in ensuring people are diagnosed early and complete the treatment. With TB, mere coverage of services is not sufficient. Quality of TB care matters, in both public and private sectors. Despite the fact that the Indian government provides TB diagnosis and treatment free of cost in public health facilities, 1.3 of the 2.8 million TB cases in India are treated in the private sector (or 2.2 out of 3.6 million according to one estimate based on private sales of TB drugs). To add a further complication, patients who either do not get the right course of treatment or do not complete it, may not only relapse and remain infectious but may also develop resistance to the most common TB drugs. Antimicrobial resistance (AMR) dramatically increases the cost of treating TB (as shown in the graphic below), and only has a 50 percent rate of success. Analyses show that AMR containment in general is a ‘hard-to-resist investment opportunity.’
Three weeks after the bold target of eliminating TB in India by 2025 was announced, India’s Revised National TB Control Program (RNTCP) published a draft of a new National Strategic Plan (NSP) for TB Elimination 2017-2025. The NSP, if approved, funded, and fully implemented represents a game change in the fight against TB in India. In addition to strengthening RNTCP to improve services and outcomes for the 1.5 million patients it treats in the public system, the Plan sets out a bold roadmap to reach out to private providers and provide support to the millions of patients treated in the private sector. Building on promising pilot results, the NSP proposes to do so by providing incentives to providers to follow standard protocols for diagnosis and treatment as well as notify cases to the government. Patients notified to the government will in turn receive a cash transfer to compensate them for the direct and indirect costs of undergoing treatment as well as incentives to complete treatment. Being notified will also allow the government to provide home visits, counseling, and implement preventive interventions.
While critics will argue that the proposals of the new NSP have risks and have never been tried at the scale that is proposed in India, the stakes are too high for business as usual approaches. Consider the toll TB takes on Indians. India accounts for 27% of the world’s 10.4 million new TB cases, and 29% of the 1.8 million TB deaths globally. TB is one of the top 5 causes of death at ages 30-69. Most TB deaths in India occur among young adults in the economically productive age group, with high economic and social costs. In 2006, TB caused India to lose an estimated 23.7 billion USD, and patients often deal with catastrophic out-of-pocket expenditure.
The cost of implementing the new NSP is estimated at USD 2.5 billion over the first three years, a steep increase over the current budget. Historically, despite being a highly cost-effective program, and despite having a high absorptive capacity, RNTCP has struggled to receive funding that is commensurate with the scale of India’s epidemic. This simply cannot continue. India must start backing its ambitions with rupees. Therefore, the real test of whether the bold plan by the Health Ministry can be implemented and the ambitious target set by the Finance Ministry achieved will be whether enough resources can be mobilized to find, treat and offer quality care to all TB patients, regardless of where they seek care.
This article was first published by Devex on 23rd March, 2017.




Join the Conversation