Nearly half of all pregnancies worldwide are considered unwanted or mistimed (Sully et al. 2020). If you think this is mainly a developing country problem, you’d be mistaken: roughly the same share of pregnancies is unintended in the United States (Bailey 2020). The term unintended is inexact: finding out that you are pregnant is not like finding out you have a dangerous heart condition: it is possible to be ambivalent about the former much more so than the latter. So, some share of the above does not constitute a problem or, at least, much less of one. But, still, lots of women, who state a clear preference, such as “I don’t want to have any more children,” or “I would like to wait at least three years (say, till I get my college degree) before having a child,” are becoming pregnant against their stated wishes. Such events are more likely among disadvantaged and underserved populations, such as younger, less educated, and poorer women.
Two main barriers standing between women and the use of effective contraception have been proposed: informational constraints and cost (Bailey 2020). Again, these are as salient policy issues in which to intervene in the United States, as they are in low- and middle-income countries. For example, the independent evaluation of the Delaware Contraceptive Access Now initiative, which tackles reimbursement policies, funding, and training for health care providers, is currently underway (expected to be completed later this year). The percentage using a long-acting reversible contraceptive (LARC) in Delaware barely reached 15% among women, aged 18-49, up from low single digits about 15 years earlier (Upstream, USA).
A recent working paper with some of my brilliant junior colleagues (Katy Bergstrom, Vitor Hadad, Luca Parisotto) and some equally brilliant senior colleagues (Susan Athey, Julian Jamison, Julius Dohbit Sama) evaluates interventions designed to address these two barriers to contraceptive uptake, using data from the pilot phase of an adaptive experiment at a Women’s and Children’s Hospital in Yaoundé, Cameroon. In today’s post, I’d like to describe the two interventions that we designed are currently implementing in our ongoing adaptive trial.
Following and during a series of workshops in different locations in Cameroon, starting in late 2017 and continuing over a two-year period, we developed a tablet-based counseling app (simply the app for the rest of this post), which is designed to be a job-support tool for health providers who conduct family planning counseling with women. The app was designed by a large and multidisciplinary working group – comprised of OB-GYNs, nurses, public health experts, and behavioral economists. Crucially, the working group included nurses, who would eventually use the app, public health officials from the Department of Family Health at the Ministry of Health in Cameroon (MoH), and researchers from our partner hospital, HGOPY. [1] The collaborative design, which combines accepted best family planning counseling practices used around the world in an attempt to ensure a high quality service while tweaking those practices to fit the local context and constraints, contributed to the usability of the app by nurse counselors. The long pre-pilot and pilot phase of our study, which allowed the providers to apply their new state-of-the-art training to counseling, allowed the counselors to get comfortable using the app and likely led to the high levels of satisfaction among clients receiving counseling (see empirical evidence on this below).
The app serves three purposes in our study:
1. A job-support tool for the nurse counselors,
2. The medium through which clients are randomly assigned to interventions, and
3. A data collection tool (via syncing anonymized data to secure cloud servers) for the trial.
The app carries out a comprehensive ‘needs assessment,’ which welcomes and assures the patient of a empathetic and confidential counseling session. Through a series of questions that structure the conversation between the provider and the client, the app then collects information on the following:
· basic demographics, birth history, and pregnancy check,
· pregnancy intentions, using a question similar to One Key Question,
· previous experience with contraception, along with preferences for particular methods,
· preferences for side effects, and
· medical history and vital statistics.
Using a simple internal algorithm that we designed, the app then uses the clients pregnancy intentions, preferences for contraception and side effects, and typical use effectiveness of each method to produce an “internal ranking” of the four modern methods of contraceptives (plus lactational amenorrhea or LAM for those who are eligible) in order of suitability for the client’s stated preferences.
[For those who are interested, it is useful to run through the app. My co-author, Parisotto, who also had a big hand in coding the app, prepared a six-minute video that you can find here: just fast forward to 18:30. You can also download slide deck from that talk here.]
The ‘needs assessment’ gives way to the ‘method choice’ section, where clients are randomly assigned to one of two different approaches to counselling: this is the first of our two interventions, which aim to take advantage of the key role default settings and choice architecture plays for decision-making in health (Johnson et al. 2005). In the control condition, which is designed to mimic the established, or status quo, approach to counseling, clients given information about all contraceptive methods and asked to choose the method they would like to discuss. The counselor is expected to provide no guidance or advice during this process: they provide neutral information about a range of modern methods and allow the client alone to decide what methods to delve into further and decide. We call this approach the “Individual Decision-Making” approach or the IDM. Crucially, in this intervention arm, the internal ranking of methods by the app is revealed neither to the provider nor to the client.
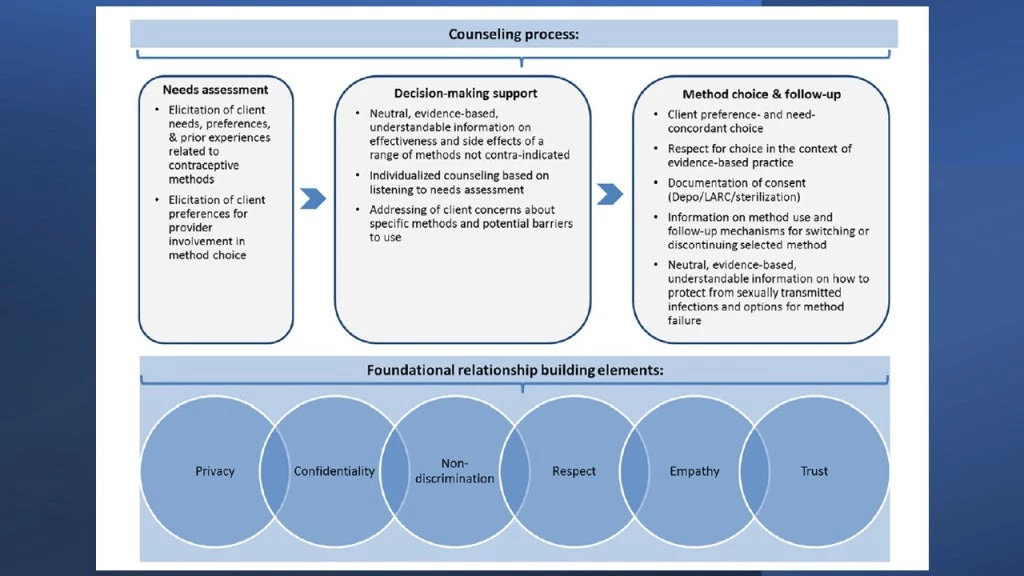
The design of the app, i.e., the counseling tool, is grounded in the quality in contraceptive counseling framework proposed by Holt, Dehlendorf, and Langer (2017) - see Figure 1 from their paper below: a needs assessment is followed by decision-making support, which leads to a method choice by the client.
In the alternative counseling approach we propose, the app reveals methods sequentially, starting from the most suitable method according to the client’s preferences towards side-effects, their fertility objectives, and the methods’ typical use effectiveness. The counselor tells the client that based on their conversation so far (i.e., the needs assessment), while there might be a number of suitable choices for her, the top-ranked method is deemed most suitable. If she’d like to discuss it, they then discuss it in detail, and she can either choose to adopt that method or ask to hear about the next method in the app’s rankings and so on – until she makes a decision. The client can, of course, rule out any method that she does not wish to discuss and move to the next one. We call this approach “Shared Decision-Making” approach or the SDM.
In the SDM approach, the counselor, with the help of the app, provides “…individualized counseling to allow room for providers to be involved in the decision-making process if individuals so desire. This is a shift away from the historical focus on an informed choice model in which individuals are given extensive information in order to make their own independent choices.” (Holt, Dehlendorf, and Langer 2017) The old and still largely prevailing informed choice model mentioned in that sentence is what our IDM approach tries to mimic, as the status quo.
However, while shifting away from individual to shared decision-making, SDM contrasts with the Holt et al. framework in one key aspect: if a client agrees to discuss the top-ranked method and chooses to adopt it, she does not get counseled on any other methods. As a detailed discussion of each modern method can take a non-negligible amount of time, a client who likes a method that is best-suited for her (according to the app, based on her elicited preferences) saves time – both for herself and for the providers, who are often busy with the next client waiting outside the counseling room. [Interestingly, as I will write next week when I discuss the evidence from the trial, SDM leads to more detailed discussion of a range of methods than IDM. As such, it improves the informational content of the counseling session in an individualized manner.] The client is, of course, provided extensive information on expected side effects, reasons to return to the provider, and the possibility of discontinuing the chosen method and switching to another one as desired. The app is designed so that if a client returns, her information from the original counseling session is quickly recovered and, if the client decides to switch to another method, the counselor can refer to the ranking of methods for the client. All removals of long-acting contraceptives are free in our study.
As can be seen from the discussion above, SDM tries to increase the uptake of the method that is most suitable for the client, minimizing the possibility of side effects and other issues and, hence, the risk of switching and discontinuation. It tries to do so in a manner that reduces/eliminates provider bias and promotes respect, empathy, and trust. If such an approach were to increase the uptake of more effective long-acting methods, such as the IUD and the implant, while causing a trade-off with client welfare or satisfaction, it would be much more questionable. Importantly, as I will also discuss more next week, follow-up surveys with clients indicate that SDM maintained respect for their autonomy in decision-making: we found no differences between the two randomized counseling arms in a checklist of quality-of-service indicators, clients’ level of satisfaction with their counseling session, or their willingness to return to the hospital for FP services in the future. These levels of satisfaction and quality of FP service delivery are very high at HGOPY, the study site.
We also have a third group of clients who were not randomized into a counselling style intervention because they expressed a strong preference for a particular method (they wanted to renew it, or already had been counselled on it) and did not want/need to sit through a full counselling session. Such clients are counseled on their preferred method first and only if there is a contraindication or the client changes her mind, then other methods are discussed. These clients are part of our randomized discount intervention but not the counseling one.
The app we developed is on a survey platform. It can be conducted in multiple languages (our nurses work in French and English, for example). It can be adapted to different contexts and the underlying ranking algorithm can be adjusted to give different weights to different aspects of the method and to incorporate other criteria not currently considered by the app (but, of course, discussed by the nurses: it is important to remember that the app is a job-support tool and not a replacement for a well-trained counselor). With some adjustments, it can also be used as an online tool for people to get a sense of their preferred options (to then discuss with their provider) or as a waiting room app on a tablet at the clinic. Please contact us if you would like to use it in your practice or as part of another study.
If you want to wait until you have seen the evidence on the relative effectiveness of these counseling approaches (and discounts, the discussion of which I also defer until next week, as this post is getting long), please be back here on Monday. Or, just read the working paper and leave questions in the comments section.
[1] The study protocols received administrative authorization from the MoH, along with IRB approvals and renewals from the “Comité National d’Ethique de la Recherche pour la Santé Humaine”, annually since 2018. The study is registered at clinicaltrials.gov (NCT03733678) and the AEA RCT registry (AEARCTR-0003514), where a pre-analysis plan for the adaptive trial can be found.


Join the Conversation