 A digital-in-health approach can help put patients and communities at the center of the HIV response. Copyright: World Bank
A digital-in-health approach can help put patients and communities at the center of the HIV response. Copyright: World Bank
Outstanding work by researchers, policymakers, medical professionals, and, most importantly, affected individuals and communities has made great progress. For those with access to medicines, HIV is no longer a death sentence. And the HIV response has been a trailblazer for a new, intensified, and integrated approach that has helped reshape pandemic response and the face of public health. Despite this progress, serious inequalities remain.
Integrating technology in the fight against HIV
We need to continue to research, provide access to prevention and treatment, and tackle stigma and discrimination. But innovation is also needed. And as the new UNAIDS report states, communities should lead the way in this work—so those closest to the challenge can quickly and powerfully learn, adapt, and act as needs and opportunities arise in today’s rapidly changing world.
In addition, technology and data are integral to daily life—and to handling crises. This is equally true in health and the society-wide fight against HIV. But current approaches are opportunistic, piecemeal, and fragmented. New thinking—a digital-in-health approach—is needed to get more value out of technology and data, ensuring systems deliver care that is accessible, equitable and cost-effective in normal times and during crises.
Lessons from COVID-19
Data from the COVID-19 pandemic spotlight the real-time power of this approach. Countries with higher levels of digital adoption pre-pandemic responded more effectively, exhibited more decisive government action, and, as a result, had fewer COVID-19 cases and deaths. Heinrichs et al. (2022) found that a country’s level of pre-pandemic digital adoption was almost as influential as demographic and lifestyle factors in predicting COVID-19 deaths and cases.
Figure 1. Links between digital adaptation prior to COVID-19 and COVID-19 cases and deaths
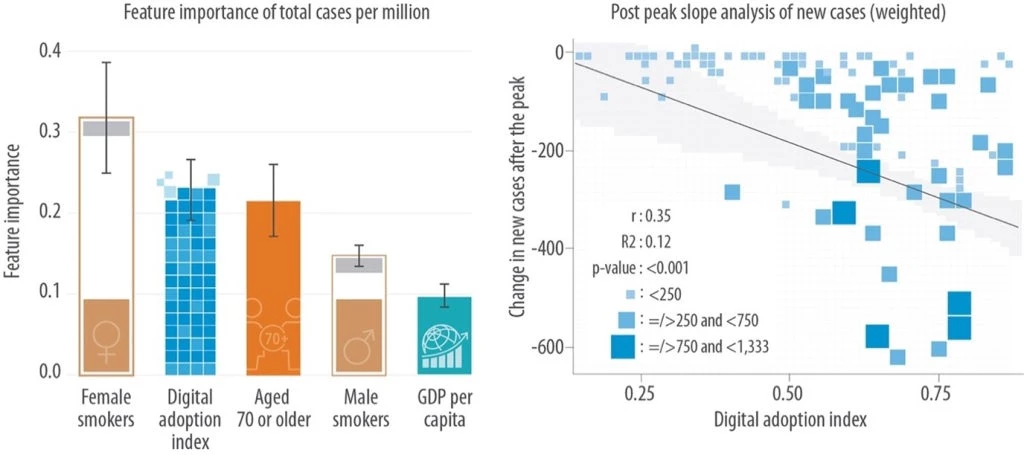
Note: Panel (a) shows that the level of digital adoption prior to COVID-19 was as instrumental in determining the total COVID cases per million population as biological determinants, such as the share of females who smoke. Panel (b) shows that countries with larger changes in post-peak new COVID-19 cases had higher levels of digital adoption prior to COVID-19.
In-country examples also support this approach. Countries that were more successful in their COVID-19 responses embedded technology and data in their health systems. Togo, for example, used digital tools to rapidly roll out emergency cash transfers to vulnerable populations and vaccinate their citizens. In Indonesia, the Ministry of Health created a digital transformation office to improve health information and digital technology certification processes.
In short, it is clear expanding digital technology should become a cornerstone of health system resilience.
These lessons and opportunities apply equally to HIV. Done right, this approach can help put patients and communities at the center. It can improve equity for those affected and vulnerable—arming them with information and tools that can empower them to lead. And it can help all involved achieve equity and integration goals in the Global AIDS Strategy.
AI for better HIV prevention
One example is artificial intelligence (AI), which a recent review by Xiang et al. (2022) found offers great promise for HIV prevention. Recent AI advances remain underleveraged, such as employing certain models to identify key individuals who can influence behavior in a community. AI can also provide real-time, analytical support to help determine appropriate community interventions.
Making it happen: Three essential areas to guide investments
Digital-in-health goes beyond the conventional understanding of digital health by integrating technology and data across health systems and the HIV response. It requires fostering trust and building capacity for digital technology use, promoting fairness, and bridging the digital chasm rather than broadening it. To do this well, as noted in a recent World Bank report on digital-in-health, countries, communities, and partners need to focus on the three key principles:
- Prioritize by choosing evidence-based digital solutions that respond to people’s needs and are equitable.
- Connect to deliver new, more, better, and seamless health services: through leadership and partnership, data governance and regulations, and filling gaps in information and digital infrastructure.
- Scale to ensure equitable access to all: improve digital skills and literacy, create synergies with wider digital transformation agendas, foster nimble public-private and private-private partnerships, and support with financing, monitoring, and implementation.
Navigating these waters will not be without obstacles. But with the right strategy, the promised value of digital technologies can be realized across the HIV response by empowering those on the frontlines, enabling community leadership, and providing powerful tools to tackle inequalities.
To receive weekly articles, sign-up here




Join the Conversation