This blog post originally appeared on the Global Financing Facility website.
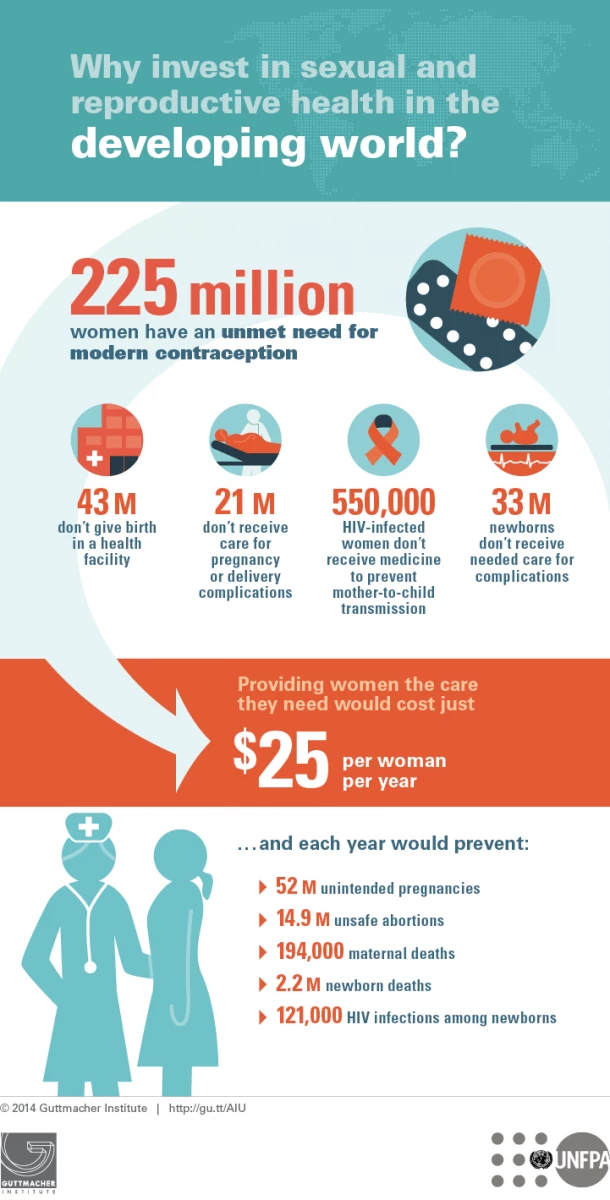
Every year, more than 200 million women want to prevent or delay pregnancy—but they’re not using contraceptives. Why?
Because many of these women don’t have access to a range of contraceptives, and are often not aware or counselled on the options available, resulting in a significant under-utilization of family planning methods in many of the countries where the demand for these services is actually high. In the Democratic Republic of the Congo, for example, just 8% of people use contraception in spite of the high unmet demand for family planning. As a result, many countries have high fertility rates: The average woman in Uganda has 6.2 children. And in some places the mothers are not much older than their children, with adolescents ages 15-19 having children. In Kenya, adolescent pregnancy is at 18%.
Many factors contribute to this situation, calling for action across the continuum of reproductive, maternal, newborn, child and adolescent health (RMNCAH). According to the Guttmacher Institute, after becoming pregnant, four in 10 women in developing countries aren’t getting four required antenatal checkups and about one-third of women aren’t delivering their babies in a health facility. There are dire, deadly consequences: In 2015, more than 300,000 women died during pregnancy, childbirth or within a few weeks of giving birth, and almost 2 million babies died in their first week of life.
Additionally, a lack of comprehensive sexuality education and access to adolescent-friendly services as well as harmful practices such as early and forced marriages, contribute to 16 million girls between the ages of 15-19 giving birth every year globally and more than 3 million of them resorting to unsafe abortions. Pregnancy-related deaths are the second leading cause of deaths in this age group, and their babies also have a substantially higher chance of dying than those born to 20-24-year-old women. Teenage childbearing results in inter-generational poverty, denying both the mother and child education and employment opportunities to make a better future.
Providing comprehensive sexual and reproductive health services—including family planning; pregnancy, antenatal and newborn care; treating pregnant women who are living with HIV; and treating sexually transmitted infections—allows women and their children to not only survive, but thrive. Maternal and newborn deaths would plummet if we fully met the need for reproductive, maternal and newborn health services. The lives saved are those of people like Rose and her baby in Samburu County, Kenya, who have a much-improved chance of surviving and thriving when they get the healthcare they need.
Because Rose and her baby survived and because Rose has access to family planning, her daughter will have the opportunity to attend school. Bringing this to scale will drive labor force participation and increase family income, all of which contributes to reducing poverty in some of the world’s poorest countries.
This transformational change is the vision of the Sustainable Development Goals (SDGs) agenda that the Global Financing Facility (GFF) in support of Every Woman Every Child is helping to bring about. The goal of the GFF is to contribute to ending preventable maternal, newborn, child and adolescent deaths by 2030 and improving the health and quality of life of women, adolescents and children. How?
The GFF is dramatically scaling up resources in 16 countries to improve the coverage, equity and quality of an integrated package of RMNCAH services that generate impact at scale, moving countries toward the goals of universal health coverage and sustainable health financing.
All of the GFF country investment cases are country-driven, prioritized and costed RMNCAH plans. Key partners come together under the leadership of the government to mobilize domestic and international resources to fund these investment cases and provide the necessary technical support and capacity-building measures to ensure that the investment cases not only support smart investments, but that they are implemented at scale and are sustainable. The investment cases are accompanied by a health financing strategy that helps direct funding for priority sexual and reproductive health, to:
- Provide sexual and reproductive health information, counseling and services, including family planning, across the full continuum of care, as part of an integrated package to improve the health of women, children and adolescents;
- Increase the availability and use of three or more high-quality family planning methods, along with the dissemination of accurate family planning information;
- Prevent and manage sexually transmitted infections and HIV/AIDS;
- Scale up the coverage, quality and utilization of cost-effective nutrition services, focusing on pregnant women, lactating women and children under 5;
- Improve and scale up the sexual and reproductive health services provided to adolescents, both within and outside of the health sector;
- Ensure reproductive health commodity security; and
- Address equity concerns in the delivery of sexual and reproductive health caused by income, geography, age, gender and other factors.
As the GFF completes its first year since the launch at the July 2015 Financing for Development conference, we are optimistic. All of the GFF-supported countries are keen to address the unfinished RMNCH agenda as well as focus on underinvested areas such as family planning and nutrition, and targeting neglected populations such as adolescents. Countries also are focusing on reducing inequities and improving quality of care in ways that are most suitable to their specific context. For example, an innovative pilot in the western highlands of Cameroon is showing promising results for improving the quality and use of maternal and child health services.
Similarly, in DRC, where maternal mortality is high, at 846 deaths per 100,000 live births, the country’s investment case is prioritizing improving the coverage of quality and equitable RMNCAH services and strengthening health management systems. Sexual and reproductive health interventions, such as family planning, are integrated in the RMNCAH package and focus on strengthening the supply and distribution of family planning inputs, integrating family planning services in postpartum care, scaling up sexual and reproductive health services at the clinical and community levels, and providing youth-friendly sexual and reproductive health services.
As Liberia recovers and rebuilds from the 2014 Ebola outbreak, the country’s investment case is focusing on integrated RMNCAH interventions in six counties with the highest burden, with a strong focus on improving the delivery of quality emergency obstetric and neonatal care.
And the government of Kenya is investing in innovative supply-side performance incentives, like those that helped to ensure that Rose and her baby got the care they needed, and demand-side vouchers and conditional cash transfers to overcome inequities, while focusing on 20 counties that have the poorest RMNCAH outcomes.
These are early days in a long journey. It is important to remember that, “ if [we] want to go fast, go alone. If [we] want to go far, go together.”



Join the Conversation