I personally felt mental health’s deep-rooted importance when I returned home to Rwanda in 1996, just after my people were traumatized by the 1994 Tutsi genocide. At a time when we needed mental health services the most, there was only one psychiatrist in the entire country.
In an act to survive and rebuild, we turned to our communities for healing. Giving a voice to the people and collectively finding a solution to the mental health challenges that we faced at that time has helped Rwanda to resiliently move forward on a path toward recovery.
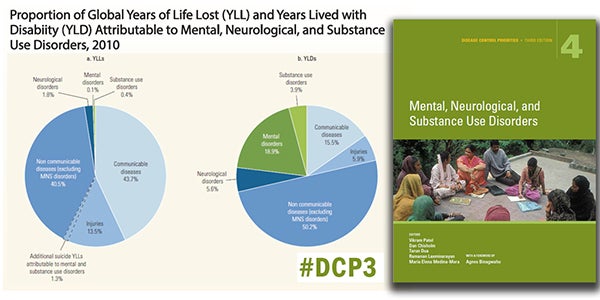
Around the world, mental health illnesses lurk in the shadows. Although they account for 10 percent of the global disease burden, they are left underestimated and unsupported worldwide.
A new book on the most effective approaches to this growing challenge is thus a welcome call to action. Mental, Neurological, and Substance Use Disorders is the fourth of nine volumes of Disease Control Priorities, third edition (DCP3), an up-to-date analysis of health interventions in developing countries published by the World Bank. In this volume, the world has in its hands a series of evidence-based approaches, cost-effective strategies, and implementation guidelines for MNS disorders.
This comprehensive review comes at an opportune time. Changing epidemiological and social determinant health profiles show the world’s readiness for sustainable development goals (SDGs) to aim for universal health coverage. We, as global leaders, have a moral obligation to advocate for comprehensive, effective services backed by human-rights-oriented legal frameworks to protect those living with MNS disorders as part of this quest toward meaningful universal health coverage. Prioritizing the supply of quality MNS services at the community level while also improving the demand for such services must come with this advocacy effort.
Although these steps may seem daunting, there is reason for hope. We can build on the lessons from the world’s 15-year fight against HIV/AIDS. Across low- and middle-income countries (LMICs) in the 1990s, both supply and demand for HIV/AIDS services were absent because there were no delivery platforms. No money or support was given to create a delivery structure. No laws were written to protect the human rights of those stigmatized by HIV/AIDS.
Today, it is a drastically different story. Progress against HIV/AIDS for the past 15 years tells us that no evidence-based, multisectoral, holistic, and rights-based approach is too sophisticated for LMICs. It demonstrates that specialized referral service systems are possible, even for one of the most complicated and stigmatized of conditions. It illustrates that as bidirectional supply and demand is created, the much-needed link between patients’ needs and an effective global care response will grow stronger.
I challenge global leaders to build upon these lessons learned from the HIV/AIDS response and apply it positively to the challenge of MNS disorders. We must no longer overlook the deleterious effects that the lack of quality MNS services has upon our communities. We should strive to build universal health care systems specifically recognizing MNS disorders’ genetic, biological, and cultural roots. And as a global community, I implore us to create enabling environments to address the social determinants of health affecting MNS disorders.
This call to action need not be answered alone; let us work together as a global team to change the status quo and demand health equity for all.


Join the Conversation