This is the eighth in this year's series of posts by PhD students on the job market.
High rates of stunting in many developing countries pose important health threats to young children and lead to adverse later-life outcomes. Many nutrition-specific interventions that target a single dimension of causes of child undernutrition have often found limited effects. This generates the question as to whether interventions that address multidimensional and nutrition-sensitive causes of undernutrition, such as lack of knowledge and income, are more effective in bringing about healthy child development.
Experimental Design and Interventions
My job market paper tests this by designing and implementing a community-based cluster randomized experiment in Ethiopia that randomly provides nutrition education in the form of behavioral change communication (BCC) and food vouchers. Specifically, we explore the effects of releasing the knowledge constraint, the income constraint, or both constraints simultaneously using three treatment arms: BCC only (BCC), voucher only (Voucher), and both BCC and voucher (BCC+Voucher) interventions for mothers with one or more children between 4 and 20 months. We target this age range because stunting prevalence increases rapidly after the first six months, as shown in Figure 1, because exclusive breastfeeding no longer meets the energy and nutrients needed for rapid child growth. We estimate intent-to-treat effects using the analysis of covariance method by controlling for the baseline value of the dependent variable.
Figure 1. Stunting Prevalence by Child Age in Ethiopia
Source: Local polynomial smoothing predictions with 95% confidence intervals estimated using the DHS data (Ethiopia DHS, 2000, 2011)
The BCC treatment was an interactive nutrition education intervention complemented by various participatory learning methods including videos and visual aids, roleplays, cooking sessions, and testimonials. We offered 16 weekly sessions that lasted about an hour. The key message was to feed infants and young children diverse and adequate diets that include vitamin A-rich fruits and vegetables and animal source foods daily. The voucher treatment provided food vouchers of 200 ETB (approximately 10 USD) per month for four months, which could be used for buying any food items at nearby markets. This amount is similar to the cash or food transfer amount of Ethiopia’s Productive Safety Net Program which was set to be about 8.5 USD at the time of the program design. The treatments were provided for four months, shorter than other BCC studies, to make the program more cost-effective for scaling up while covering all key messages for improving child feeding.
BCC improves mothers’ nutritional knowledge and a third of the vouchers are spent on non-staple food
Using BCC and voucher administrative data, we first show that the implementation went reasonably well. Mothers of both BCC and BCC+Voucher groups attended about 74% of the sessions on average and showed similar improvements in nutritional knowledge scores (Panel A of Figure 2). Knowledge did not improve for those in the Voucher group. The positive impact of BCC and the null effect of Voucher on mothers’ knowledge are comparable to other studies with longer intervention periods. Voucher recipient households redeemed about 88% of the face value of the vouchers on average, a third of which were spent on non-staple food including animal source foods and fruits and vegetables for both Voucher and BCC+Voucher groups.
Figure 2. Treatment Effects on Knowledge and Child Dietary Diversity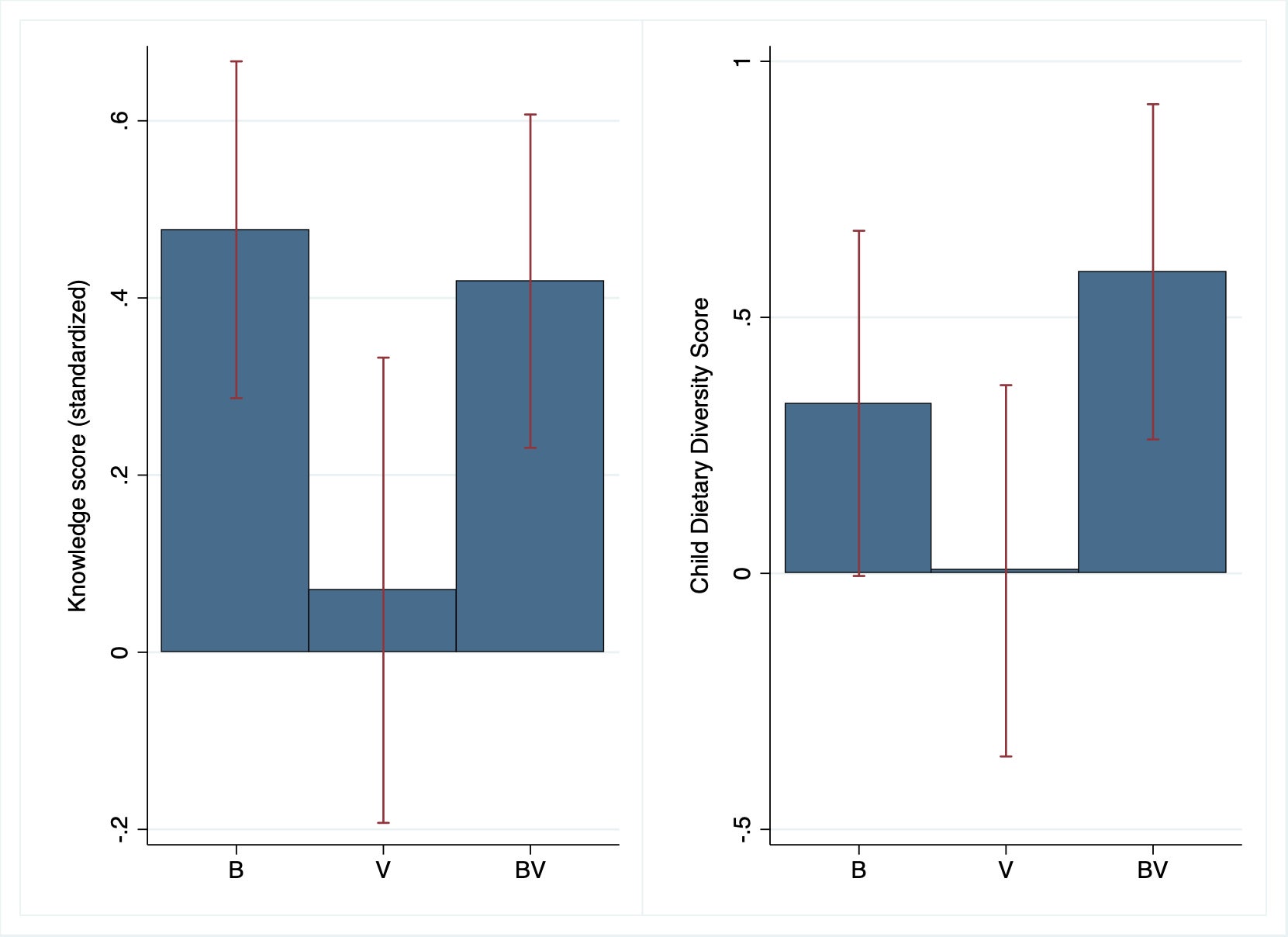
Note: The bar graphs represent coefficient estimates of intent-to-treat effects and the red vertical lines indicate 95% confidence intervals. B=BCC, V=Voucher, BV=BCC+Voucher.
BCC+Voucher has the greatest impact and BCC has some impact on improving child diet quality, while Voucher has none
We then look at the treatment effects on mothers’ child-feeding behaviors, reflected in the quality of children’s diets. We find the greatest improvements in child dietary diversity score in the BCC+Voucher group and some improvements in the BCC group, but none in the Voucher group (Panel B of Figure 2). This pattern is consistent across a number of other child diet quality measures we examine including the proportion of children who meet the WHO’s minimum dietary diversity, meal frequency, and acceptable diet standards, with the impact size of BCC+Voucher being almost double that of BCC. For few specific behaviors with which there is little or no cost associated—e.g., adjusting the age of introducing complementary food—we find that BCC alone could bring about similar improvements to BCC+Voucher. However, Voucher had no effect on mothers’ child-feeding behaviors, except that they (mis-)perceived that their children had better quality diets than other children.
BCC+Voucher leads to stunting reduction by preventing stunting from occurring among at-risk children
Given the changes in child diet quality, we further investigate the treatment effects on children’s physical growth and stunting in particular. Figure 3 presents height-for-age Z scores (HAZ) across the study arms at baseline and follow-up.
Figure 3. Distribution of Height-for-age Z Score (HAZ) at Baseline and Follow-up
Note: This figure presents kernel density graph of height-for-age Z scores of eligible child at baseline (Panel A) and at follow-up (Panel B). The red vertical line represents -2SD, below which means stunted growth, an indicator for chronic undernutrition.
First, without any treatment, we find that the overall HAZ decrease over the 6-month-period between baseline and follow-up (Figure 3). Similar to the pattern among children over 6 months in many developing countries, stunting prevalence increased rapidly from 28% to 42% in the control group from baseline to follow-up. Amid the rapidly increasing trend of undernutrition, we find stunting reduction in the BCC+Voucher group by 9.8 percentage points at least in the short-run, but not in other groups. Figure 3 further illustrates that the lower tail of the HAZ distribution of BCC+Voucher shifted rightward rather than the upper tail from baseline to follow-up. This means that the BCC+Voucher treatment was particularly effective in improving diet quality for those who are otherwise more prone to be chronically undernourished. Moreover, Figure 4 shows that BCC+Voucher prevented stunting from occurring during the critical age range from 12 to 18 months rather than reversing it. For children not stunted at baseline, the BCC+Voucher group has lower stunting prevalence at follow-up (19%) than the control group (33%). However, for children stunted at baseline, stunting prevalence at follow-up is similar between BCC+Voucher and control.
Figure 4. Stunting Prevalence at Follow-up by Baseline Stunting Status
Note: The bar graphs represent mean stunting prevalence at follow-up by study arm conditional on whether stunted at baseline. The red vertical lines indicate 95% confidence intervals. B=BCC, V=Voucher, BV=BCC+Voucher, C=Control.
Are knowledge and vouchers complementary?
Lastly, our study design allows us to address the important question of whether the effects of the multifaceted treatment are additive or synergistic (complementary), which other similar approaches—e.g., poverty graduation programs, among others—have not been able to disentangle. We find that the large impact of BCC+Voucher is driven by complementary effects of BCC and vouchers, indicating that the impact of the sum (BCC+Voucher) is greater than the added impacts of the parts (BCC and Voucher). We find some evidence of complementary effects on child-feeding behaviors, while the greatest complementary effect is exhibited in child growth and stunting outcomes.
Policy implications: Address both constraints simultaneously and target all children at 6-18m
For social protection or nutrition programs aiming to reduce child undernutrition, providing nutrition education and income simultaneously may be most effective. Also, when implementing programs similar to BCC+Voucher, it may be best to target all infant and young children in the critical age range of 6 to 18 months, rather than targeting only the already undernourished children or a broader age range because BCC+Voucher is particularly effective in preventing stunting from occurring in this age range rather than reversing it.
Seollee Park is a PhD Candidate in Applied Economics at Cornell University.



Join the Conversation