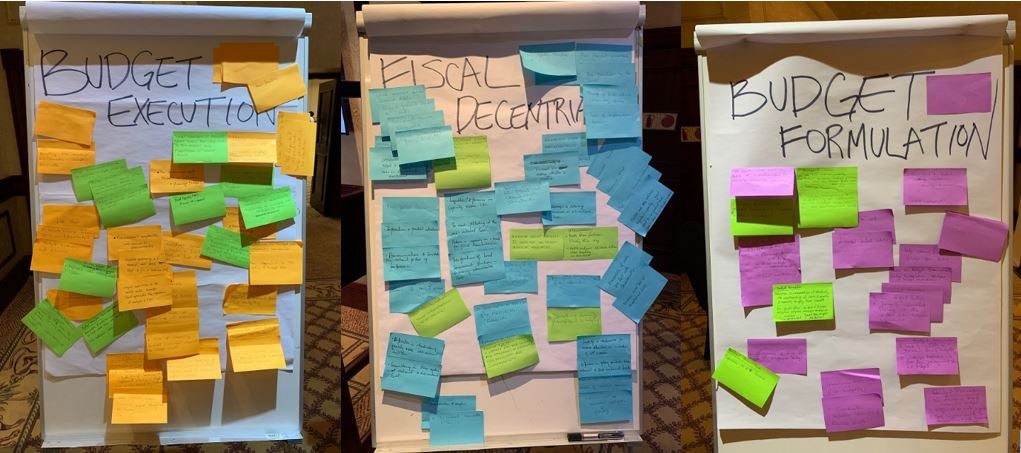
 Examples of participants diagnostics and proposed solutions
Examples of participants diagnostics and proposed solutions
Hamilton vs Jefferson, or Treasury vs Congress
The U.S. public financial management (PFM) system evolved out of various controversies. One of these controversies was a dispute between Alexander Hamilton and Thomas Jefferson about how much discretion the executive branch of the U.S. government should exercise over the spending of public funds. Jefferson’s victory enabled Congress to assert its authority by making appropriations so highly specific as to hinder executive action. Had Hamilton won, the Executive would have attained extraordinary budgetary powers – an arrangement similar to that in some of our client countries today.
“Should health facilities retain the fees they collect?”; “Should service delivery and procurement be decentralized?”; “How does program budgeting improve service delivery?” These are all public financial management (PFM) questions raised by participants at a recent workshop held in Gaborone, Botswana focused on PFM in health services delivery. For the workshop, a World Bank team invited counterparts from ministries of finance, health and from local governments across the region. The goal of the workshop was to create a shared understanding of PFM challenges in health service delivery, draw lessons from the regional reform experience of counterparts, and to identify opportunities for further reform.
How to improve PFM in health—Some lessons learned
Let’s go back to the introductory question about how flexible the budget execution should be: how much control should, for example, a Ministry of Finance exercise? In the health sector, an important PFM challenge is to balance fiscal control with the necessary flexibility for effective service delivery. This tension also surfaced during the workshop: representatives from Ministries of Finance took the position that prudent fiscal management was critical; service delivery practitioners on the other hand argued that autonomy and flexibility is necessary to react to rapidly changing needs in the sector. Virements, which are transfers of budgetary resources between programs, policy areas, and/or expenditure categories, could improve the situation at the margins, but providers and spending units should in general adhere to original plans.
A lesson learned from the workshop is that this conundrum could be overcome through a risk-based approach to control. Such an approach would differentiate high value from low value transactions and help public financial managers create an environment where flexibility is granted without giving up control where it is necessary. For example, in the case of Tanzania, 85% of transactions make up just about 10% of the budget volume. For these numerous small transactions, greater flexibility could be allowed. On the other hand, the 15% of transactions that make up the remaining 90% of the budget volume would benefit from the given control protocols. For Tanzania and potentially other countries in the region, the switch to a risk-based approach and the higher flexibility for small transaction could allow facility managers to provide more responsive service delivery to the population. This approach has since been documented in a recent World Bank working paper.
More questions raised than answered—What’s next?
The above flexibility vs control discussion was but one of many exchanges among workshop participants. Practitioners from across sectors worked together at eye level to map out the sets of PFM issues affecting their countries. It emerged that countries in the region are dealing with similar difficulties. However, countries differ greatly in how they deal with the difficulties. Examples include innovations in the fintech sector in Zambia to digitize facility payments to suppliers and strengthen facility autonomy; mainstreaming PBF reforms into general budget management in Zimbabwe, Zambia, and Lesotho; introducing PFM reforms in Malawi that finance facilities directly; or addressing the retention of user fees in Namibia and Eswatini.
The next step is to enter in-depth discussions about how to implement more such potential solutions. Having created a shared understanding of PFM challenges in health service delivery, the foundation for overcoming this next challenge has been laid.
The conference was conducted under the Health Financing in Southern Africa (South Africa, Namibia, Zambia and Eswatini) ASA and kindly sponsored by Southern Africa CMU.



Join the Conversation