 Admission department in Kisumu hospital, Kenya
Admission department in Kisumu hospital, Kenya
What can Kenya do to make further strides on its quest toward Universal Health Coverage (UHC) and achieving upper-middle income country aspirations?
Over the past years, Kenya has accelerated progress toward Universal Health Coverage, both in terms of expanding coverage of quality health services and reducing financial hardship. For example, Kenya’s life expectancy increased from about 51 years in 2000 to about 66 years in 2018 while the incidence of catastrophic health spending decreased from almost 13% in 2013 to 8% in 2018.
In December 2017, the President of Kenya unveiled UHC as one of the key Big 4 Agenda of his administration. The Government of Kenya undertook various reforms and increased the allocation of resources from both national and county governments to the health sector to finance the ambitious agenda.
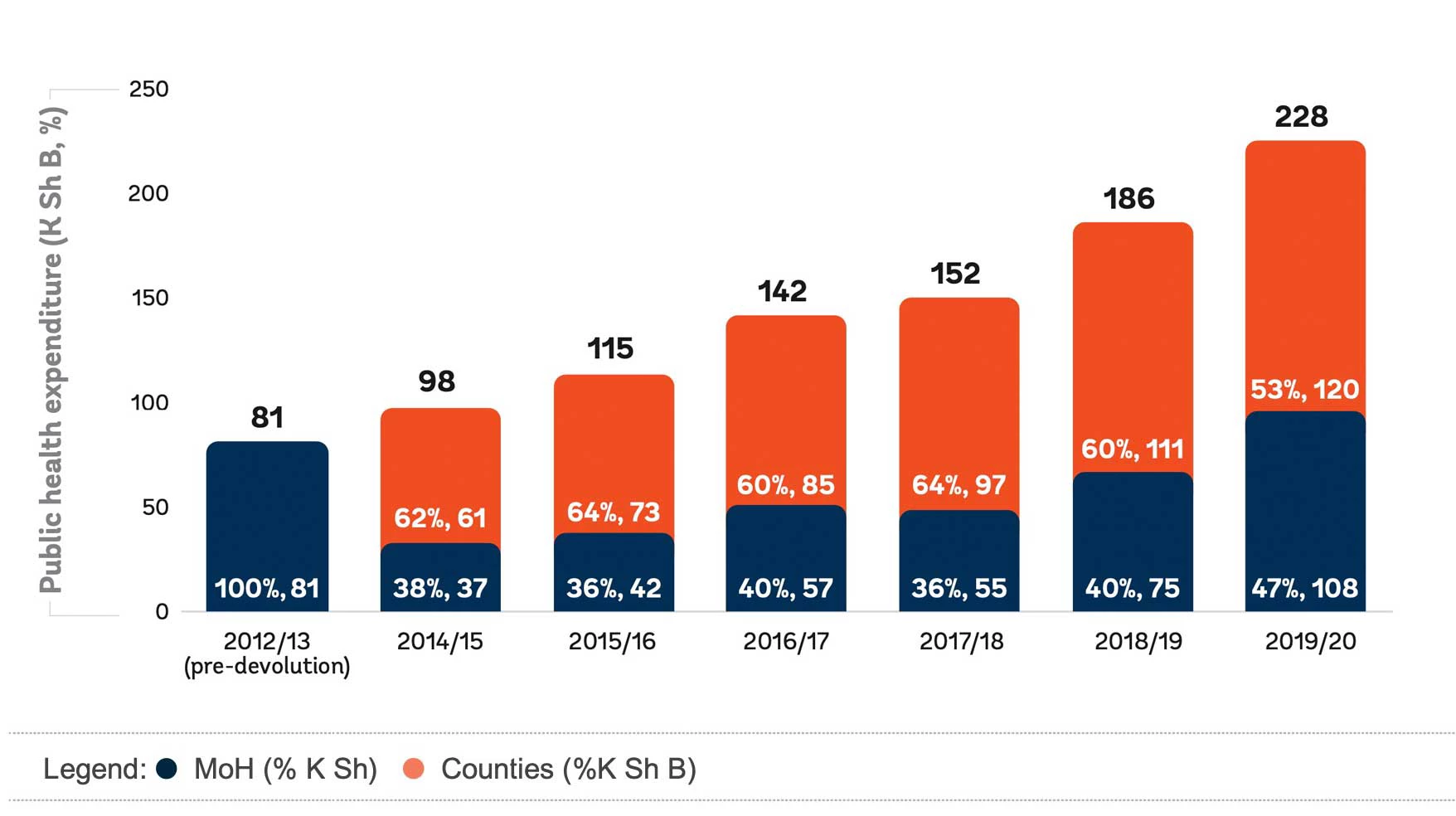
Public Health Expenditure by Level of Government (K Sh Billion, in Nominal Terms)
and as Percentage of Total Government Health Expenditure (Percent)
However, the crisis resulting from the COVID-19 pandemic is expected to negatively impact progress toward UHC. Firstly, Kenyans sought less care during the pandemic, which is expected to have negative impacts on service coverage. Secondly, the expected limited fiscal space means that the increase in resources to finance the expansion of UHC in the coming years might also be limited.
In the short term, it will be critical for the Kenyan government to preserve spending on health, and as the economy and available resources grow, the country may return to increasing spending on health. In the meanwhile, Kenya ought to focus on maximizing the impacts of current public spending - improving the efficiency, the effectiveness and equity of its public investments.
Our recently published Public Expenditure Review for Health in Kenya sheds light on the performance of public spending on health vis-a-vis the UHC objectives set by the government and provides concrete recommendation on how Kenya can further improve results. We share a few of these below:
- Concerted efforts are needed to tackle the largest sources of inefficiency within the health sector and increase the value for money of public spending. This includes, among others, prioritizing quality primary health care services rather than highly specialized health services at the hospital level and reducing input related inefficiencies, especially in terms of availability and competencies of human resources for health, medical equipment, and medical supplies.
- The move from coverage to effective coverage will require improvements in the quality of care. The Kenyan government should create an appropriate framework to incentivize and monitor health workers to be present at health facilities and deliver quality services to patients. HRH skills and capabilities could be increased by moving towards competency-based training models, support professional development and equip health facilities with adequate medical supplies and equipment that allow providers to do their job well.
- Continue prioritizing investments in disadvantaged geographic areas and population groups to further narrow socio-economic inequalities alongside efforts to expand UHC. Collecting and monitoring data disaggregated by socio-economic characteristics coupled with further expansion of programs to support vulnerable and disadvantaged population groups, including through the expansion of health insurance subsidies and coverage of essential medicines, will be essential to make further strides on the reduction of inequality and inequity in the country.
- Improve monitoring and governance systems to accelerate progress toward upper-middle income countries health targets. This could include further strengthening and institutionalizing the annual sector review both at the national and the county level and increase investments in health management and information systems that can generate timely and useful information for planning and budgeting, monitoring of performance monitoring, and overall benchmarking.
- Consider introducing reforms to accelerate the flow of resources to front line facilities and strengthen the linkages between payment and performance/achievement of results. The national government should work with the county governments to explore potential PFM related reforms that could be implemented to ensure conditional grants flow directly to health and other frontline facilities, rather than cascading slowly and irregularly through the different layers of the intergovernmental financing framework.




Join the Conversation