 Solomon Islands’ National Referral Hospital in the capital, Honiara
Solomon Islands’ National Referral Hospital in the capital, Honiara
“We don’t have enough money to achieve our targets” is a common refrain in many offices, particularly around budget time. But is it always true? And when limited financial resourcing is available, how do you prioritize one need over another? These questions have certainly been asked within Solomon Islands’ Ministry of Health and Medical Services (MHMS) as it works towards the goal of Universal Health Coverage.
To help find some of the answers, the MHMS requested assistance from our team at World Bank to help map national health spending against health indicators, so that officials could see how their use of resources relates to outcomes for patients. The goal has been to help the Ministry make better decisions about where limited funding is allocated, and help them prioritize resources across the many divisions and programs delivered through Solomon Islands’ health system, to ensure the best health outcomes for the country.
Identifying gaps in the system
Our team’s work began in early 2020, with one of the first insights to emerge being that while some divisions and programs had extensive indicators, others had none. Without indicators, it was difficult to measure programs’ and divisions’ performance, and therefore work out whether resources were being used effectively. However, now that these indicator gaps have been identified, MHMS can focus on ensuring all divisions and programs have appropriate indicators to which their performance can be measured in the future.
Increased spending doesn’t always improve outcomes
The analysis also highlighted that spending more money doesn’t always produce improved health outcomes. For example, despite increases in spending to curb the spread of malaria across the Solomon Islands, there has, sadly, been little improvement in malaria incidence rates over the last five years. Furthermore, there were instances where funding for health promotion in schools had been reduced; yet the health promotion outcomes had continued to improve.
To be clear, we certainly don’t advocate, in any way, for reducing health spending. However, this point has helped to emphasize the importance of ensuring spending is as effective and impactful as possible.
Better informed resource allocation
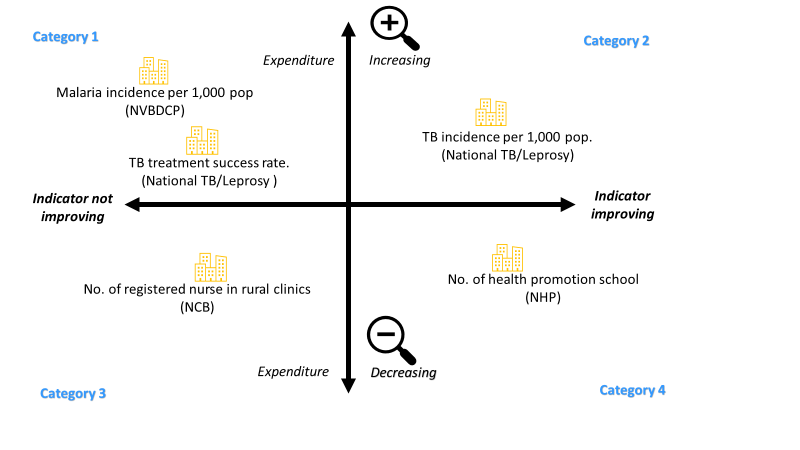
By classifying indicators into four different categories (see Figure 1, below), senior officials were better able to consider options for resource re-allocation during the Ministry’s annual budget process.
The goal was to see that in the future, all program and divisions would operate in either category 2 or 4 where health outcomes and indicators were showing improvement. Then, once indicators were improving, to see how resources could be more efficiently utilised and managed to avoid over or under spending at the expense of maintaining good health outcomes (especially in resource limited settings).
| Figure 1:
Acronyms in Figure 1 NVBDCP – National Vector Born Disease Program NTP – National TB and Leprosy Program NNB – Nursing Council Board NHP – National Health Promotion National TB/Leprosy – National Tuberculosis/Leprosy division |
Challenges and opportunities
We encountered several challenges during the study, with both presenting opportunities for strengthening health system management. One challenge was the difficulty in finding reported data for some of the indicators, including who was responsible for their monitoring and reporting. In the future it would be beneficial if an appropriate division or position be identified to maintain data collection and reporting on the indicators the MHMS needs to report on.
Another challenge was working out how effectively financial resources were being used by small units within the larger divisions. The small units often had their own unique indicators, but their budgets were tagged at the divisional level which made it hard to work out how much they were spending to achieve their own specific outcomes. More detailed monitoring of costs for these units in future can help address this issue.
More efficient use of existing resources
One limitation of the study was that we looked only at health spending and linked this to health outcomes. Of course, other factors such as human resource capacity, infrastructure, medical equipment, and technology also influence health outcomes. Given this, we caution that the findings of this study should be interpreted with that limitation in mind.
Nevertheless, the study has certainly highlighted that increasing financial resources is not always the solution to improving health outcomes. It makes little sense when programs showed increasing financial resources and yet worsening indicators and health outcomes. In these situations, and in exploring ways to improve; efforts could be better spent investigating the efficient use of existing resources. This would certainly help Solomon Islands move closer along the path to Universal Health Coverage; something that all Solomon Islanders deserve.
This work was supported by the Australian Government, through the World Bank-managed Advance Universal Health Coverage Multi-Donor Trust Fund. This fund aims to drive more equitable expansion of Universal Health Coverage in Solomon Islands and 12 other countries across East Asia and the Pacific. It is funded primarily by the Australian Government, in collaboration with GAVI, The Global Fund, and the Bill and Melinda Gates Foundation.


Join the Conversation