 woman receiving vaccine injection in arm
woman receiving vaccine injection in arm
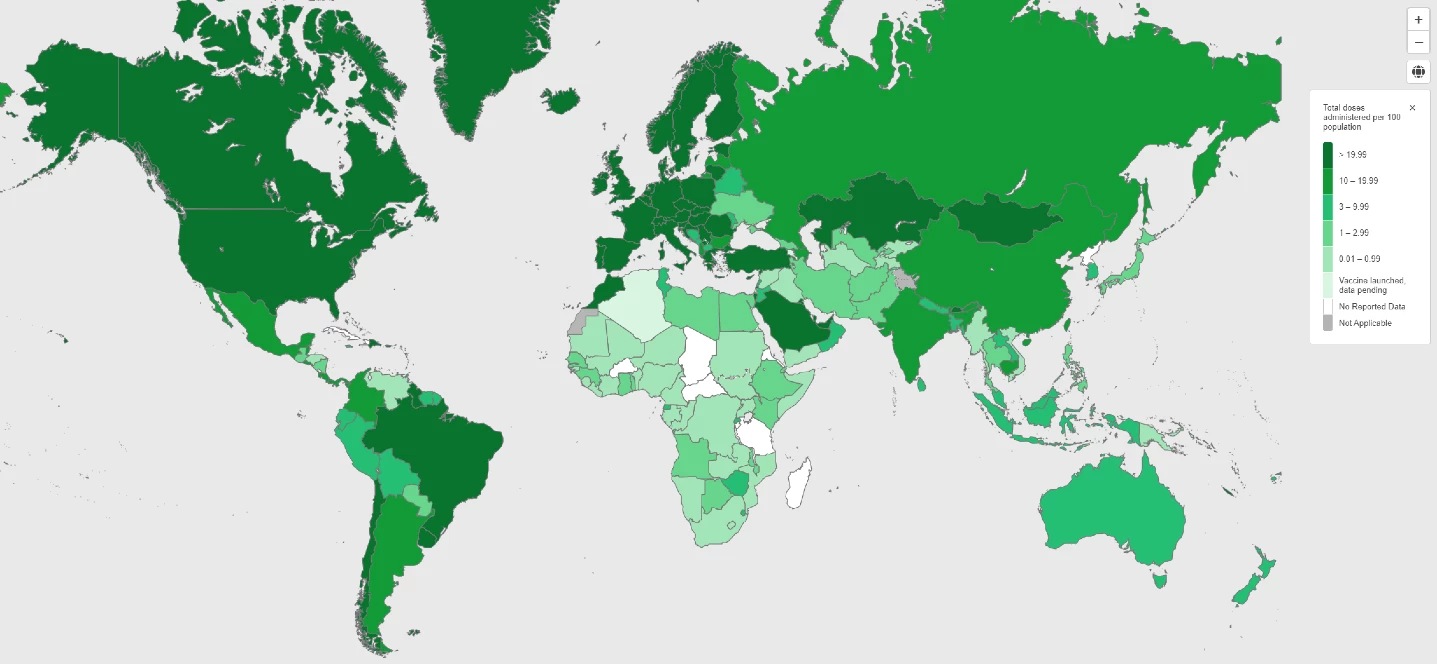
Vaccine rollouts are underway in over 181 countries and territories worldwide, yet only a handful of Sub-Sahara African (SSA) countries have started vaccinating their population. Regional access to vaccines is hindered by a worldwide shortage of vaccine production capacity, a race for quick vaccine access by richer countries and a lack of local resources.
If developing countries are unable to vaccinate their population against COVID-19, the global economy stands to lose as much as US$9.2 trillion, according to a study commissioned by the International Chamber of Commerce (ICC) Research Foundation.
The World Bank Group (WBG) has already committed more than $108 billion to help countries recover from the health, economic and social impact of the pandemic. This includes US$12 billion financing to help countries purchase and distribute vaccines, tests and treatments and strengthen their vaccination systems.
What are the costs for Sub-Saharan Africa?
Estimating the costs of COVID-19 vaccine deployment enables countries to plan and budget for its distribution. African countries are seeking vaccines through different channels, including the COVID-19 Vaccines Global Access (COVAX) Program, the WBG’s US$12 billion financing package, the African Union (AU), bilateral negotiations, and donations.
Figure 1: COVID-19 vaccine doses administered per 100 people
Under COVAX Advance Market Commitment (AMC) to support high-risk populations in low- and middle-income countries, 41 SSA countries will have access to 600 million free, safe and efficient COVID-19 vaccine doses, estimated to cover 20% of their population by the end of 2021. The AU will potentially bring an additional 20% of vaccine coverage to the region. The Bank Group’s financing will further allow more than 30 African countries to expand their vaccine pools and strengthen national health systems. However, countries’ ability to purchase enough vaccine to protect their entire population will depend on their economic capacity.
How much would it cost each government?
As part of the Inter-Agency COVAX Costing Group, the World Bank is helping countries to estimate the cost requirements of their COVID-19 vaccination programs. With Bank guidance, the costing exercise also facilitates a conversation around a sustainable COVID-19 program and health system.
The information below provides preliminary estimates for countries that need tools to prioritize and advocate for the expansion of health financing for vaccines.
Table 1 shows assumptions and conditions for each cost component for countries among the COVAX AMC92 vs. non-AMC eligible countries. Given the high uncertainty associated with vaccine development and production, estimates of vaccination costs for the region are based on certain assumptions such as the parameters of coverage, availability of COVAX subsidized doses for AMC countries, pre-estimated costs per dose and general unit costs. They cover five elements—vaccine package, supply chain, climate-friendly cold chain, service delivery, and vaccine wastage—and do not include buffer stocks, labor, and capital costs.
Table 1 Vaccination Costing Estimates Assumptions and Conditions
| Category |
Vaccines (Doses only) |
Vaccine package Additional Vaccine costs |
Transport (freight and transport cost until arrival in country airport) |
Supply Chain (costs for cold chain equipment, vehicles, transport and fuel) |
Climate-Friendly Cold Chain (additional costs on top of supply chain component – inflated costs) |
Service Delivery (costs for program management: supervision and monitoring, training, social mobilization and disease surveillance) |
Wastage (vaccines discarded, lost, damaged or destroyed. Included in the ‘vaccine’ component) |
| AMC92 Eligible Countries |
Full 20% coverage by COVAX (zero cost to Gov’t) |
20% coverage costs covered by Gov’t; estimates differ by GAVI, non-GAVI etc. |
Additional 20% for climate-friendly cold chain |
20% coverage costs covered by Gov’t; estimates differ by GAVI, non-GAVI etc. |
We use an average of 5% of vaccine costs |
||
| $7 per dose, two doses needed/person; $7 price/dose recommended for COVAX (low estimate is $3/dose ; high is $8.5/dose) |
|||||||
| Non-AMC92/ Self-Financing Countries |
Full 20% coverage costs covered by Gov’t |
20% coverage costs covered by Gov’t; estimates differ by GAVI, non-GAVI etc. |
Additional 20% for climate-friendly cold chain |
20% coverage costs covered by Gov’t; estimates differ by GAVI, non-GAVI etc. |
We use an average of 5% of vaccine costs |
||
| $10.55 per dose, two doses needed/person |
|||||||
Sources: UNICEF, WHO, COVAX Costing Group
The cost of achieving herd immunity
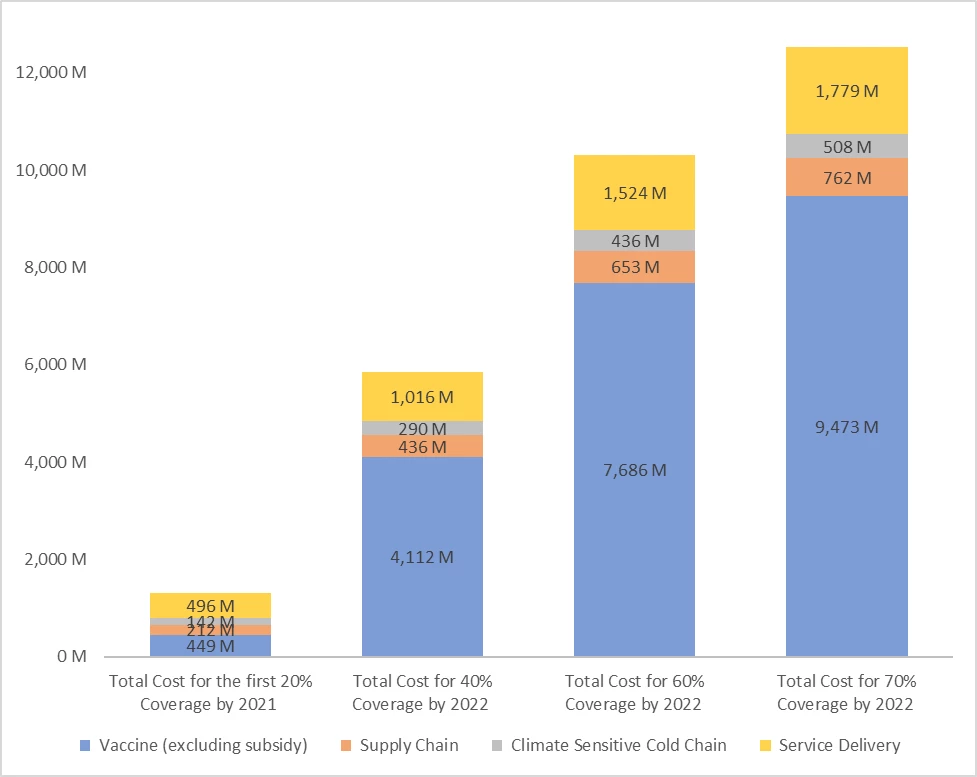
Three policy-relevant coverage cost scenarios show the extent of additional resources that SSA countries will need to cover vaccination costs. Estimations apply to the cost of vaccinating 20%, 40%, 60%, and the global target of 70% of the population. COVAX is set to provide low- and middle-income countries with enough vaccines to cover at least 20% of their population. However, countries will have to mobilize more funding to fill the gap between the first 20% and additional coverages.
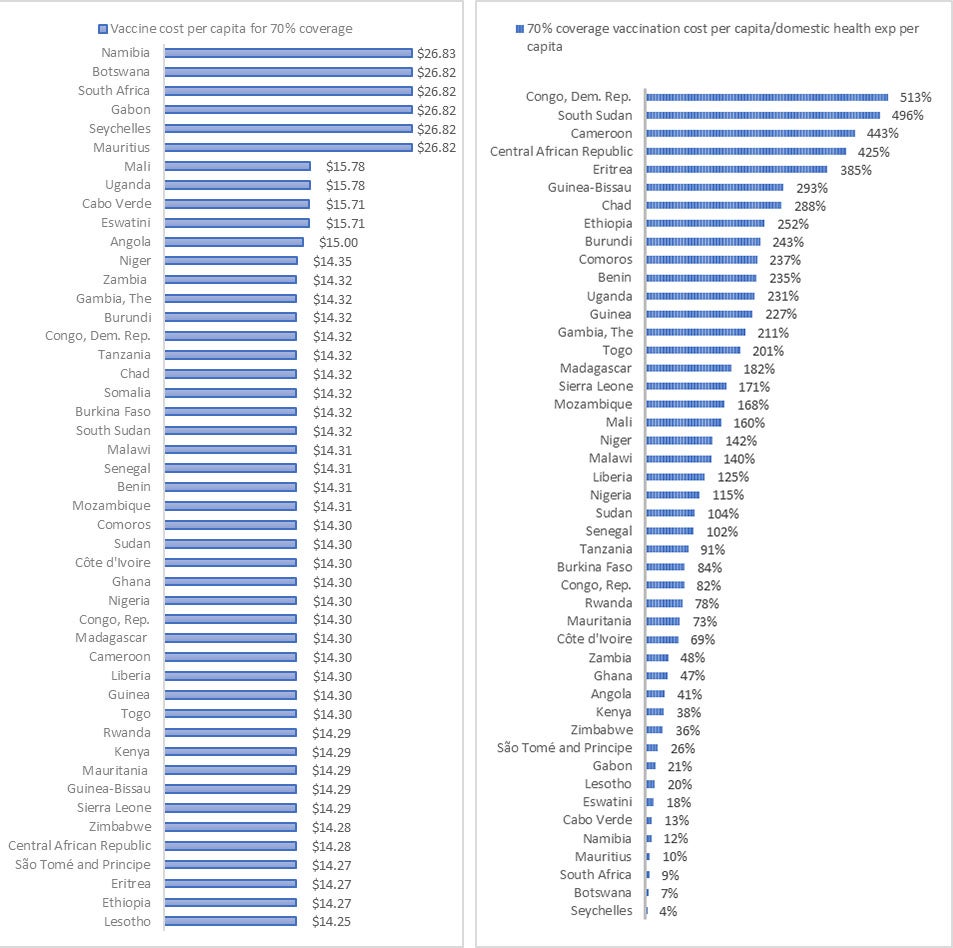
These scenarios examine the financial burden on national governments to achieve 70% vaccination coverage. In addition to $9.5 billion for vaccines, 48 SSA countries will require $762 million for supply chain, $508 million for climate-friendly cold chain, $1.8 billion for service delivery (Figure 2). The total of $12.5 billion amounts to approximately $15.17 per person in the region, with variations ranging from $26.83 for Namibia to $14.25 for Lesotho (Figure 3). The difference is mostly driven by population numbers and COVAX financing for the AMC92 countries. For simulation purposes, estimates were performed at 20, 40, and 60%, which have a total financing from the government of $1.3 billion, $5.9 billion, and $10.3 billion, respectively.
Figure 2 Total Financing Needs Estimates for SSA by Components and Coverage
Insurmountable financial burden for countries alone
To understand what this means for African countries, these average vaccination costs per capita add up to approximately 150%, or 1.5 times, the annual total government health expenditure (THE-G) per capita of African governments, although figures vary greatly among countries. These estimates also show, however, that achieving herd immunity in African countries would cost just over 1% of the potential $9.2 trillion loss to the world economy if developing countries cannot vaccinate their population.
Figure 3 shows that fiscal burdens are highest in the Democratic Republic of Congo (vaccination cost per capita is 5.13 times higher than THE-G per capita), South Sudan (4.96 times higher), and Cameroon (4.43 times higher), while in the Seychelles (0.04 times), Botswana (0.07 times), and South Africa (0.09 times), vaccination makes up the lowest share of total health expenditure.
Figure 3 (a) vaccination cost per capita for 70% coverage; (b) vaccination cost per capita/total government health expenditure
Funds are urgently needed to finance vaccination and fill the economic gap. Most SSA countries lack the financial resources to fund it on their own. Considering the economic and health losses caused by the pandemic, achieving herd immunity through equitable COVID-19 vaccination will be a good investment in the long term. Thus, robust economic mobilization and quality of spending will be determining factors.
SSA countries should consider ways to reprioritize their health financing by focusing on innovative strategies for the implementation of their National Vaccine Deployment Plans. They could explore alternative financing efforts such as additional taxes, external assistance, and/or borrowing.
Working closely with the international community will be critical to mobilize resources and vaccine donations, and apply relevant mechanisms to drive vaccine prices down. Through its financial commitment, the WBG is already extending its support to African countries to address some of these needs.
Now is the moment for international partners and African governments to step up and greatly accelerate vaccine access and distribution. With recent COVID-19 surges in several countries, we must redouble efforts now. A coordinated and well-resourced global response will provide a strong foundation to make health systems and immunization programs stronger –and more resilient for years to come.




Join the Conversation