 Many countries in Africa allocate limited resources to primary health care, but there are strategies governments can employ to increase investment. Copyright: World Bank / Vincent Tremeau
Many countries in Africa allocate limited resources to primary health care, but there are strategies governments can employ to increase investment. Copyright: World Bank / Vincent Tremeau
The COVID-19 pandemic has brought to light the critical need for Sub-Saharan African countries to prioritize investment in primary health care to develop a robust and resilient health care system capable of successfully combatting infectious diseases. Strong primary health care systems in nations like Japan, South Korea, and Vietnam may have contributed to their ability to respond to the pandemic quickly and efficiently. In administering public health activities, particularly in the fight against infectious diseases, primary health care is essential.
Health spending in primary health care in Sub-Saharan Africa remains low
Unfortunately, many countries in Sub-Saharan Africa allocate limited resources to primary health care. Most countries in the region allocate less than 5% of their GDP towards primary health care (Figure 1).
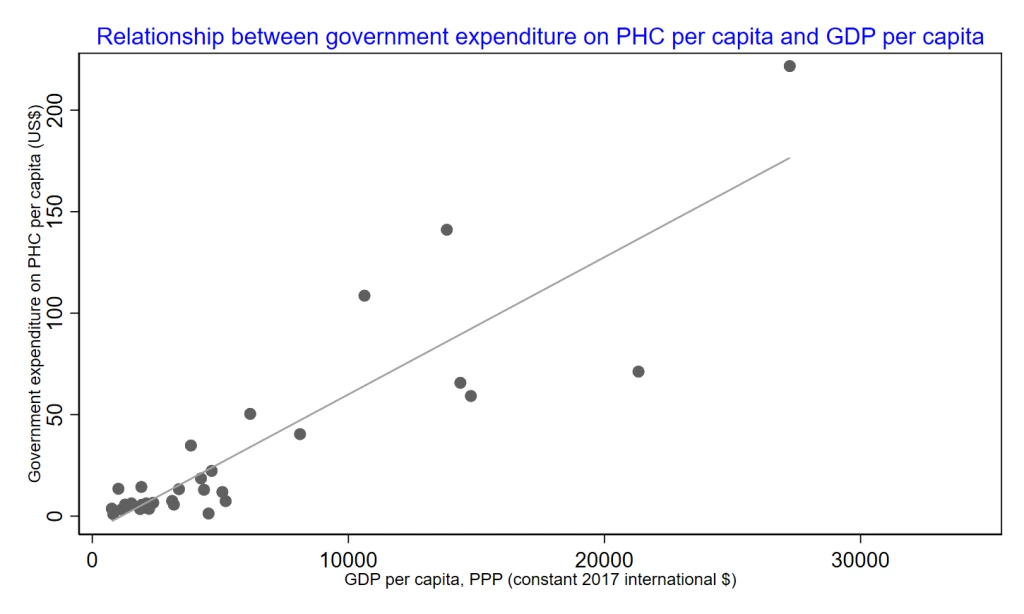
Similarly, in terms of per capita government expenditure on primary health care, countries belonging to the Southern African Development Community exhibit a higher level of investment. Notably, Seychelles stands out with the highest per capita expenditure on primary health care, reaching $222. When the countries are analyzed based on their income levels, wealthier nations such as Seychelles, South Africa, Mauritius, and Namibia commit more resources to primary health care (Figure 2).
Figure 1: Domestic primary health care financing in Sub-Saharan Africa
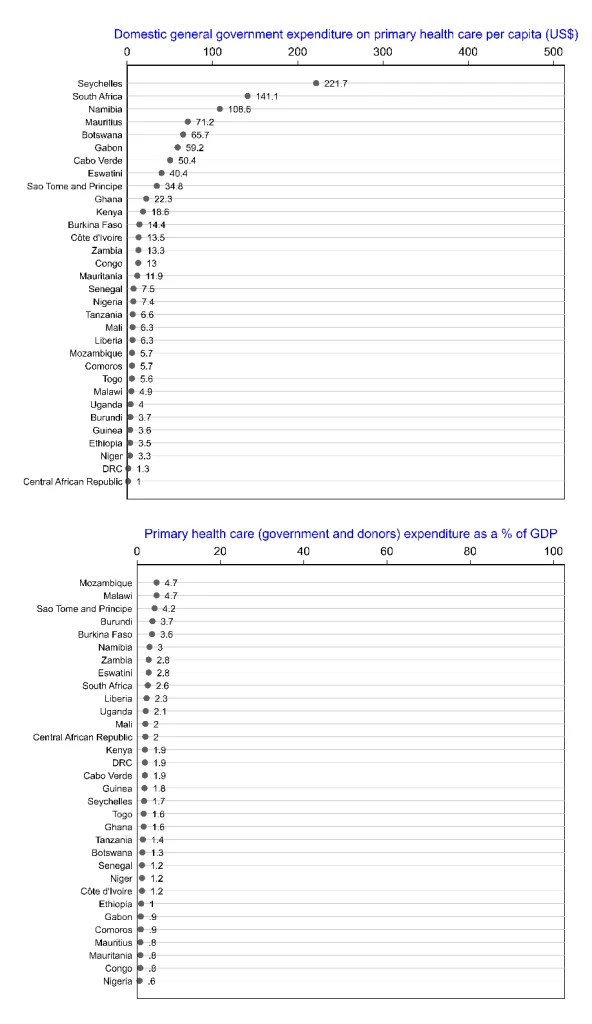
Figure 2: Examining the link between domestic general government expenditure on primary health care per capita and GDP per capita
There are various strategies that governments can employ to increase investment in primary health care, aiming to enhance its resilience to future pandemics. Here are a three potential approaches:
1. Increased funding
Policymakers have the opportunity to allocate a greater share of their budget to primary health care, specifically focusing on cost-effective interventions—immunization, task-shifting from doctors/nurses to community health workers—that offer substantial value for the resources. This entails identifying interventions that provide the best health outcomes relative to their costs. It is imperative for policymakers to prioritize health spending and guide their countries towards a pathway that is resilient to pandemics.
Policymakers could implement innovative financing mechanisms. For example, considering that the majority of countries in the region have not yet achieved the minimum recommendation set by the World Health Organization (WHO) on tobacco taxes, there is room to generate substantial funding for primary health care through increased taxation on tobacco products.
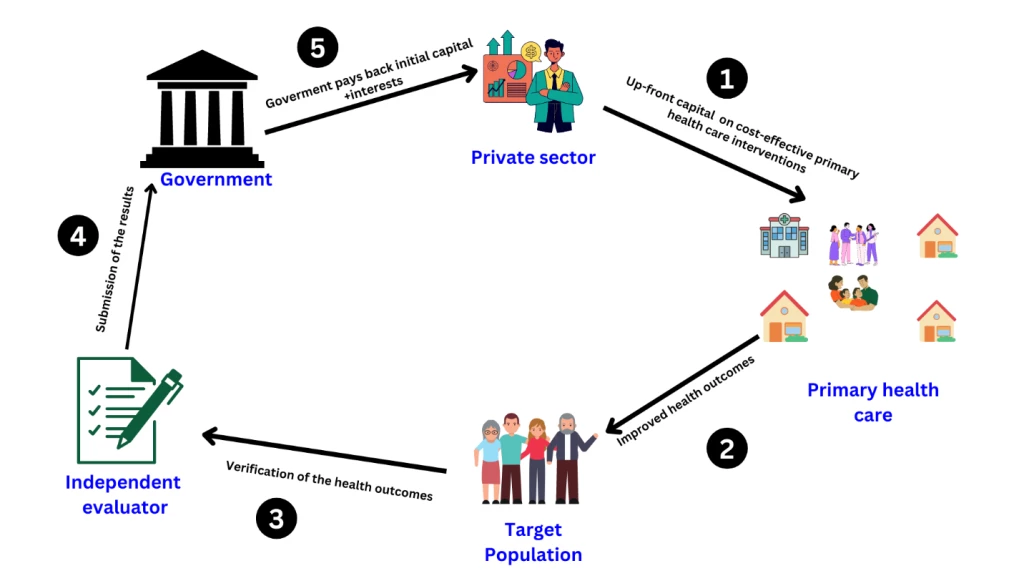
Additionally, governments can bring in the private sector, leveraging their expertise and financial support to strengthen primary health care. Enhancing collaboration with the private sector can be facilitated through the utilization of a primary health care bond, a type of social impact bond that seeks to enhance primary health care services.
In this model, the private sector contributes initial funding for cost-effective primary health care programs, and service providers implement these programs to attain predetermined outcomes. If the desired outcomes are achieved (verified by an independent evaluator), the government reimburses the investors with a financial return. These types of bonds encourage innovation, and efficiency, while also attracting private-sector investments. By issuing a health impact bond, policymakers could tap into private sector resources and expertise, channeling them towards targeted primary health care projects or programs.
Figure 3: Simplified illustration of a primary health care bond
2. Workforce development and infrastructure
A resilient primary health care system requires a skilled workforce and adequate infrastructure. Community health workers (CHWs), who play a critical role in delivering primary health care services, could receive necessary training and support. Furthermore, investments in laboratories and early warning systems could further enhance the effectiveness of the primary health care system, enabling better preparedness and response to future pandemics.
3. Digital health
Sub-Saharan African countries have witnessed a remarkable leapfrogging effect in technology. This presents a distinctive opportunity for investments in primary health care, as digital health solutions could be harnessed to overcome geographical obstacles and enhance service delivery.
Mobile applications, telemedicine, and health information systems could enhance health care accessibility, and strengthen health data management. This integration of technology can foster trust and confidence among citizens in health care providers. Furthermore, leveraging digital solutions could facilitate the enrollment of citizens in the national health insurance scheme, streamline electronic medical records, simplify service reimbursements for health care providers, and ensure the continuity of essential health care services during pandemic. Lastly, implementing an electronic surveillance system can greatly support the 7-1-7 approach (7 days to detect, 1 day to notify, and 7 days to respond) for disease surveillance, enabling efficient monitoring and response to health threats. Nevertheless, it is essential to establish effective governance in order to guarantee the protection of data privacy and the implementation of regulatory frameworks necessary for the advancement of digital health.
To receive weekly articles, sign-up here




Join the Conversation