The Government of Lesotho has spearheaded several innovations in health. These innovations have been translated into more health service utilization that might have contributed to the improvements in some health outcomes.
In 2016, Lesotho was the first adopter of the World Health Organization’s new slogan “Test and Treat” against HIV/AIDS in Sub-Saharan Africa, making it easier for people testing positive for HIV to immediately be enrolled into treatment regardless of their immunity level. The country benefitted from the US Millennium Challenge Corporation funding to rebuild all primary healthcare centers and refurbish many district hospitals, improving access to health for many Basotho, including in the rural areas. In 2008, Lesotho declared no user-fee for primary healthcare and much lower user-fees for other levels of care. Performance-based financing, an innovative financing system aligning public funding to the quantity and quality of delivered health services (as opposed to a mere budget financing inputs), shifted policymakers’ attention to delivering quality of care to the beneficiaries.
As a result, health care utilization increased. For example, the percentage of women delivering at the health facility increased from 59% in 2009 to 89% in 2018 as suggested by the latest households’ survey. In the same timeframe, utilization of modern contraceptive methods improved significantly from 46 to 65%. Child immunization coverage with basic vaccines has gone up from 62 to 69%. Last births for which women received a postnatal check within two days after birth at the facility jumped from 15 to 65%.
Have these changes and improved service utilization translated into better health outcomes? The answer is yes. Fertility, maternal, neonatal, and infant mortality rates, and HIV/AIDS incidence improved over time. The table below provides more details in the progress made for key health outcomes in Lesotho.
Progress of Key Health Outcome Indicators
| Indicator | Baseline | Latest | Direction |
|---|---|---|---|
| Human Capital Index 1/ | 0.34 (2010) | 0.40 (2020) | ↑ |
| Total fertility rate, per woman/1 | 3.9 (2009) | 3.3 (2018) | ↑ |
| Maternal mortality (per 100,000 live birth) 2/ | 579 (2014) | 544 (2017) | ↑ |
| Infant mortality (per 1,000 live births) 2/ | 71.6 (2014) | 68.1 (2019) | ↑ |
| Incidence of HIV (per 1,000 uninfected population) 2/ | 8.9 (2014) | 6.4 (2019) | ↑ |
| Incidence of tuberculosis (per 100,000 people) 2/ | 579 (2014) | 544 (2017) | ↑ |
| Survival Rate from Age 15-60/1 | 0.349 (2010) | 0.523 (2020) | ↑ |
These outcomes have improved even more rapidly among poor people. When comparing ratios of health outcomes among the richest and the poorest over time, they all move upwards towards one - indicating that such outcomes among the poorest have been improving more rapidly than among the better-off. The richest-poorest ratios moved from 0.63 to 0.66 for neonatal mortality; from 0.73 to 0.80 for infant mortality; from 0.76 to 0.90 for under-five mortality, and from 0.33 to 0.42 for fertility.
Notwithstanding the progress, Lesotho health outcomes still remain among the worst in the Africa region, signaling that the country has a long way to go to improve them. At the same time, better outcomes could be achieved by improving the efficiency and effectiveness of spending.
What can explain that contrast?
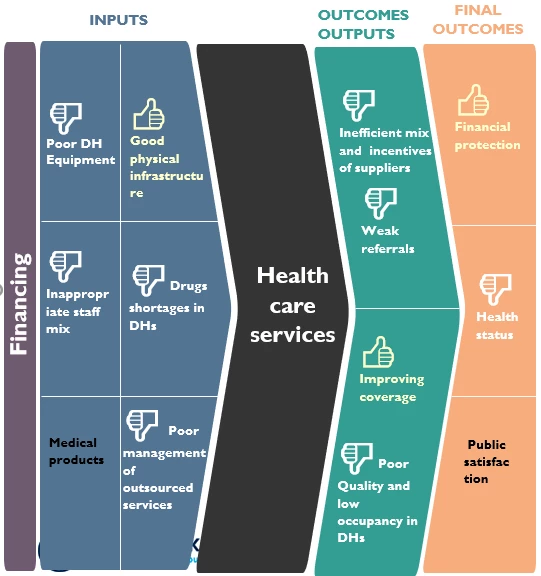
Looking into the health system both at the central and the service delivery (or district) levels, the service delivery chain faces multiple challenges.
At the central level, the government has chosen to outsource a large share (around half of the health budget) of health services to non-governmental suppliers but has not improved capacity to manage them, which remains low. Oversight of these health services’ suppliers is handled by two staff in the department of the Ministry of Health (MoH), leading to delayed payments, poor monitoring and poor accountability. The MoH has a high share of non-essential staff (such as clerks and drivers), while many essential health staff positions remain unfilled, signaling poor human resources management and inefficient use of resources. In fact, about one-third of employees at the Ministry are clerical personnel and drivers, while technical staff such as doctors, nurses, pharmacists, laboratory staff are in serious shortages, from one-fifth to three-fourths gaps.
At the district level, contravening the requirement of entry into the healthcare system through a referral system, many care seekers go directly to the referral public-private partnership (PPP) hospital in Maseru, which is a tertiary care facility and not necessarily the right level of care for the patients. While their behavior may be justified by their demand for better quality of care, this increases the cost to the Government a lot: the Government must pay for all patients as per the PPP agreement, no matter the severity of their health condition. As a result, District Hospitals’ beds remain poorly filled at 32% of their capacities, whereas the PPP hospital is frequently overwhelmed with beds occupancy at 75%. Below is a more comprehensive snapshot of the inefficiency chains in the health sector in Lesotho.
Snapshot of the inefficiency chains in the health sector in Lesotho
What can be done?
At the central level, strengthening contract management capacity with legal, finance, clinical supervision and economics expertise would result in better health care services, service providers will be made accountable for delivering on their contracts and they will be paid on time. A thorough review of the MoH’s staffing plan and prioritizing the hiring of essential medical staff would enhance the adequacy of staffing in the Ministry.
At the district level, building, strengthening, and sustaining an enforced referral system would limit care seekers from going directly to the PPP hospital in Maseru, and thus improve utilization of the district hospitals bed capacity. Also, the government could pursue its effort for quality improvement in district hospitals and health centers so that beneficiaries can gain back confidence in the quality of care, alleviating unnecessary cost from the often unnecessary use of the only tertiary health facility in the country.
Implementing these measures would allow Lesotho to gain higher value-for-money from the investments in health, while improving service delivery.



Join the Conversation