 A new report provides recommendations for processes countries can use to develop fair and equitable health financing policies. Copyright: World Bank
A new report provides recommendations for processes countries can use to develop fair and equitable health financing policies. Copyright: World Bank
In many developing countries health financing is not only inefficient and insufficient, it’s inequitable: People in developing countries pay over half a trillion dollars annually out-of-pocket for health services, which pushes about 100 million people into extreme poverty each year.
Policies regarding who contributes and how much, how resources are pooled to spread financial risk, what services are guaranteed to all, and how to purchase health services, can significantly reduce these inequities and bring countries closer to universal health coverage (UHC).
But the very process of improving such policies toward more equity and fairness can also lead to fairer outcomes and better governance overall.
Fair processes for equitable health financing
This is the topic we delve into in a new report written by the World Bank, the Norwegian Institute of Public Health, and the Bergen Centre on Ethics and Priority Setting. We also provide recommendations for the process countries can follow in developing fair and equitable health financing policies.
The Open and Inclusive: Fair Processes for Financing Universal Health Coverage report makes a case that procedural fairness plays a critical role for countries committed to UHC because it can contribute to more equitable outcomes, strengthen the legitimacy of decision processes, build trust in authorities, and promote the sustainability of health financing reforms.
To facilitate this, the report describes key health financing decisions —decisions, for example, with an impact on equity in service coverage and financial protection – where questions of procedural fairness need to be considered.
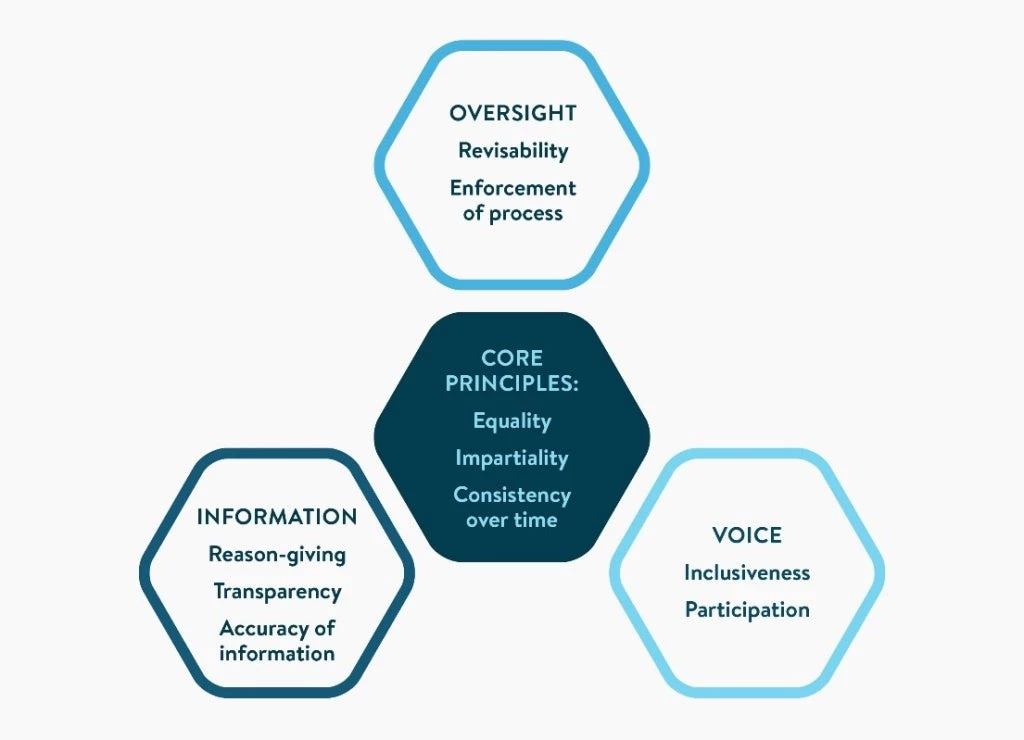
It then derives three guiding principles for the assessment of procedural fairness: equality (e.g., in access to information, opportunities to express views and to influence decisions), impartiality (e.g., ensuring that vested interests do not unduly influence the decision), and consistency over time (e.g., rules and procedures for decision making are stable over time and predictable).
Assessing procedural fairness in health financing decision-making
To facilitate the practical application of these principles, the report outlines criteria that can be used to determine if the procedures for making health financing decisions in any setting are fair.
These are organized into three domains (Figure 1). Information, the first domain, relates to open decision-making, covering reason-giving, transparency, and accuracy of information. The second domain, voice, includes participation and inclusiveness, creating opportunities for the public to express opinions and perspectives. Oversight, the third domain, includes revisability and enforcement of fairness criteria and the resulting decisions.
To illustrate how these criteria can be applied in practice, the report presents a range of country experiences in developing health financing policies, cutting across revenue generation, pooling, and purchasing.
Figure 1: Principles and operational criteria of procedural fairness
For instance, Ethiopia and Thailand use organizational arrangements that require public participation on different decision-making bodies, as well as capacity-strengthening instruments such as civil servant training for generating and using evidence.
Overall policy directions vs. technical decisions
The report recognizes that the criteria need not be applied with the scope and intensity to all types of health financing decisions. It distinguishes between decisions that set the overall directions of health financing policy (e.g., whether to introduce social health insurance on top of a tax-financed system) and more technical decisions (e.g., whether new medicines should be publicly funded, taking into account data on their safety, effectiveness and costs). Indeed, many countries ensure more extensive public participation—one of the fairness criteria—for decisions about policy directions, leaving narrow technical decisions to experts.
In cases where more limited public participation is justified, procedural fairness can be enhanced by strengthening other criteria such as reason-giving, transparency, and accuracy of information.
For example, if decisions regarding the public financing of new medicines rely on recommendations from technical experts, it is crucial that the reasons and underlying evidence supporting the acceptance or rejection of these medicines be made transparent and open to public scrutiny.
Towards a fairer process
Equity (fairness) in UHC outcomes is critical. This report suggests that procedural fairness involved in making these decisions is equally important. Even with limited resources, a growing number of countries are taking steps towards implementing a fairer process for decisions in health financing. Governments, civil society, and international partners can work in complementary ways to apply these principles and criteria and improve procedural fairness, and through this, equity on the path to UHC.
You can download the full report here.
To receive weekly articles, sign-up here





Join the Conversation