
This is a companion blog to the series of blogs from the 2016 Edition of World Development Indicators. It is a guest contribution from colleagues involved in the Lancet Commission on Global Surgery
Around the world, more than two-thirds of people still cannot access safe, affordable surgical and anesthesia care when they need it. The impact of surgical disease is not trivial; 30 percent of the world’s burden of disease is estimated to be caused by conditions requiring the care of a surgeon. Such conditions are estimated to cost low- and middle-income countries up to USD 12.3 trillion in lost economic output by 2030. Moreover, 81 million individuals face financial ruin due to expenses incurred while receiving surgical care each year.
The delivery of surgery is critical for the realization of many of the Sustainable Development Goals: Good health and well-being (Goal 3); No poverty (Goal 1); Gender equality (Goal 5), and Reducing inequalities (Goal 10).
Describing access to surgery as a treatment modality or platform of care, with relevant country-level data requires a rigorous deconstruction of the components of access upon which national governments can intervene. To this end, Dr. Jim Kim challenged the surgical community in 2014 to develop surgical indicators, along with “time-bound targets” to which the world can aspire.
Six core indicators of surgical system strength
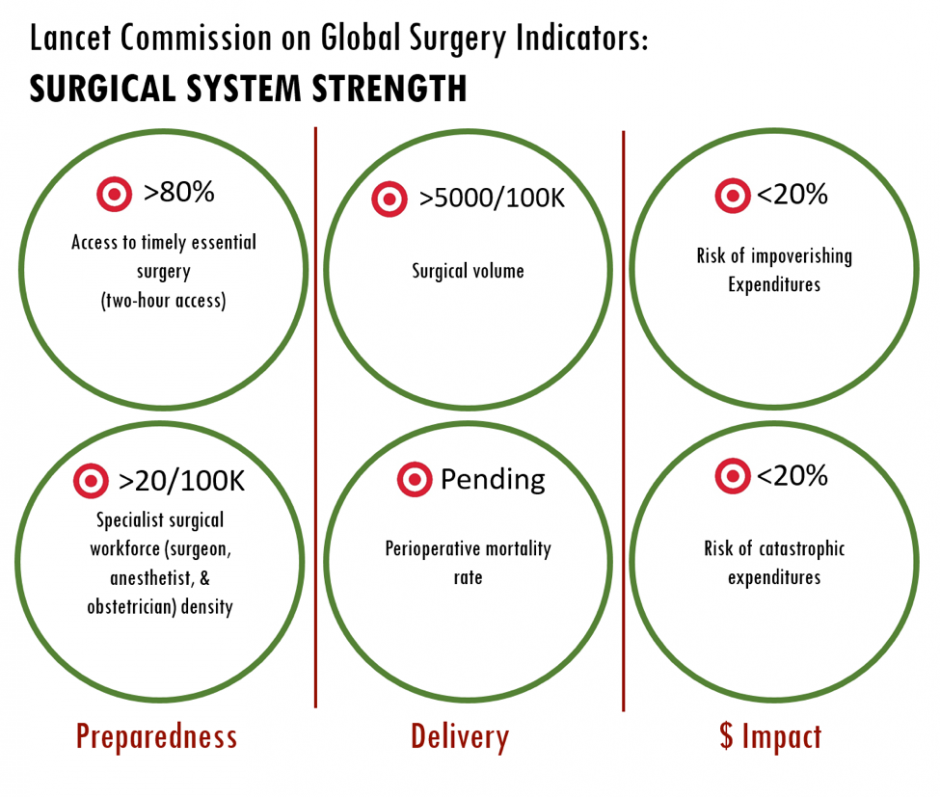 A representation of the Lancet Commission on Global Surgery six core surgical indicators
A representation of the Lancet Commission on Global Surgery six core surgical indicators
The Lancet Commission on Global Surgery, assembled in 2013 to assess surgical care around the world, responded to this challenge. Commissioners engaged in an iterative global consultative process with partners in over 110 countries to develop six core indicators of the strength of a surgical system. Two indicators assess a country’s preparedness to deliver safe surgery and anesthesia, two assess the current delivery of safe care, and two assess the state of financial risk protection for those seeking surgery, using the World Bank’s Universal Health Coverage paradigm. These indicators are:
1. Access to timely essential surgery: The proportion of the population in each country that can reach, within two hours, a facility capable of providing caesarean section, laparotomy, and treatment of open fracture (the Bellwether Procedures).
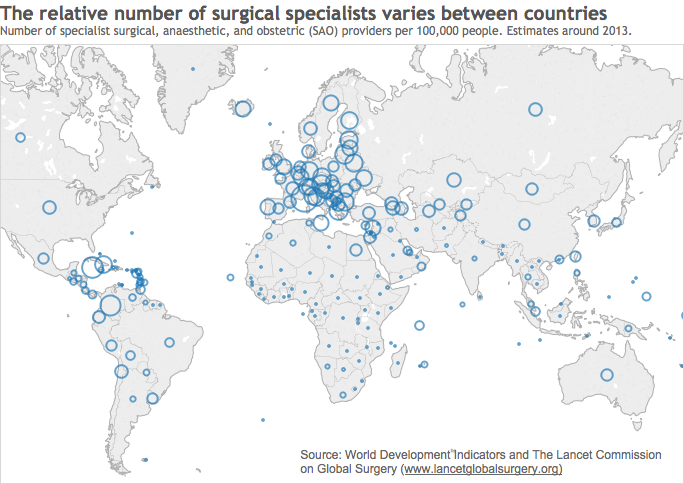
2. Specialist surgical workforce density (WDI Indicator SH.MED.SAOP.P5): The number of specialist surgical, anaesthetic, and obstetric (SAO) providers who are working in each country per 100 000 population.
3. Surgical volume (SH.SGR.PROC.P5): The number of procedures undertaken in an operating theatre per 100 000 population per year in each country. A procedure is defined as the incision, excision, or manipulation of tissue that needs regional or general anaesthesia, or profound sedation to control pain.
4. Perioperative mortality rate: The number of in-hospital deaths from any cause in patients who have undergone a procedure done in an operating theatre, divided by the total number of procedures, presented as a percentage.
5. & 6. Risk of impoverishing (SH.SGR.IRSK.ZS) and catastrophic (SH.SGR.CRSK.ZS) expenditure for surgical care: The probability of experiencing impoverishment (using a threshold of $1.25 PPP/day) when surgical care is required and the probability of experiencing catastrophic expenditure (10 percent of total income) when surgical care is required.
This minimum dataset was designed to provide essential information for ministries of health without imposing an onerous burden of data collection and analysis. While modeling exercises had provided global estimates of workforce, volume, and financial risk by the time the Commission was published in April 2015, country-level data had not yet been developed.
Alongside its academic partners, the Commission launched its Global Indicator Initiative in June 2015 to collect primary country-level data for each indicator and provide modeled data where this was not possible. Holmer, et al, provided a WHO-sponsored primary dataset of specialist surgical workforce density. Weiser, et al, developed a model providing country-level surgical volume,
Less than 10% of the surgical procedures required to save lives and prevent disability are currently performed in low-income countries
Tukey boxplot of surgical volume according to income group, with LCoGS target of 5000 indicated
In low-income countries, median surgical volume was 424.5 surgical procedures per 100,000 population, a number far short of the target of 5,000 recommended by the Lancet Commission on Global Surgery.
Specialist surgical workforce density is correlated with life expectancy
SAO density versus life expectancy. Two Commission benchmarks, 20/100,000 and 40/100,000 indicated. Bubble size represents country population
A marked correlation is seen between specialist surgical workforce density and life expectancy. Most countries with a life expectancy over 70 have an SAO density above the Commission benchmark of 20 per 100,000 population, though we undoubtedly have much to learn from the countries that achieve this life expectancy with fewer surgical specialists.
Four out of five people in low-income countries are at risk of financial ruin if they need surgery
Risk of impoverishing expenditure in the event that surgical care is required, at the country level, by World Bank Income Group
In the world’s poorest countries, over 80% of individuals face impoverishing expenditure (being pushed below the poverty line) if they need surgery, thanks to the direct medical expenses of surgery alone. The World Bank has set an ambitious goal of 80% health coverage for basic medical care by 2030; to achieve this, we must invert the current coverage ratio for surgical care in the next 15 years.
Simple tools can show within-country disparities in geographic access to surgical care
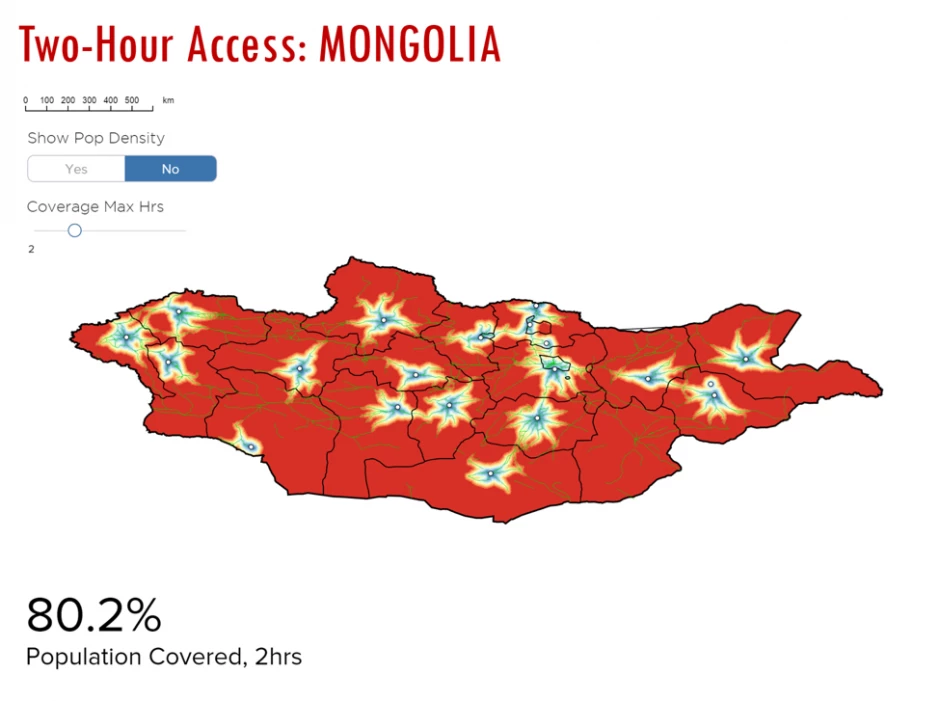
Access to timely essential surgery and perioperative mortality rate were not populated with sufficient data to be included in this release of the World Development indicators. However, the collaboration between the Commission and partners at Stanford University and Redivis brought about the creation of an automated tool to map surgical facilities and calculate population travel times to these locations.
The future of surgical data
The search continues for ever more accurate, ever more granular primary data to describe surgical care. Sustaining surgical data collection over the course of the SDGs and beyond will require the engagement of academics in all countries and the convening power of international organizations such as the United Nations and WHO. The latter has taken a central role in the collection of SAO data through its regular health workforce reporting mechanisms. Finally, through the Global Indicator Initiative, the Commission strove to engage those whose ownership of the data matters most: national ministries of health. It is our hope that this engagement will allow ministries to thoughtfully adopt this data in developing policy toward universal access to safe, affordable surgical and anesthesia care when needed.





Join the Conversation